You’ve probably heard about electrolytes from advertisements for popular sports drinks. And it’s true – high performing athletes do lose electrolytes during activity that need to be replaced.
But electrolytes are important for all of us, athletes or not. From a nutrition standpoint, electrolytes are just as important as protein, fat, carbohydrates, and vitamins. Without electrolytes, we wouldn’t be able to get all the benefits of other nutrients.
In this blog I’ll share more about what role electrolytes play in the body, how pregnancy impacts electrolyte needs, and ways you can increase your electrolytes.
What are electrolytes?
In the context of nutrition, electrolytes are essential minerals that carry an electric charge once dissolved in fluid. Sodium, potassium, chloride, calcium, and magnesium all act as electrolytes. You find them in all bodily fluids — such as blood, sweat, urine, cervical fluid, and amniotic fluid — where they play a myriad of functions.
Electrolytes are necessary for keeping your heart beating normally which keeps your energy levels up. They support adrenal health, fluid balance, and may help prevent common annoyances like headaches and cramps. This means that getting enough minerals in your diet is very important.
Electrolytes & Pregnancy: Why do we need more electrolytes during pregnancy?
In pregnancy, fluid volume increases by as much as 50% and this gradual increase starts fairly early in the first trimester. Not only does blood volume increase, but as baby grows and your uterus expands, amniotic fluid accumulates in the uterus where it:
- Cushions baby
- Supports lung development (baby is breathing in amniotic fluid, which has hormones, nutrients, and antibodies)
- Maintains a consistent temperature
- Supports their developing digestive system
- Assists in nutrient delivery and the excretion of wastes
- Helps baby’s skeletal and muscular system develop (amniotic fluid provides the right amount of room for baby to move and kick/punch the walls of the uterus to stimulate muscular growth and bone density)
Outside of these pregnancy-specific roles, adequate fluids allows for maintaining good circulation, provides shape and structure to every cell in your body, helps regulate body temperature, and aids in the digestion and absorption of nutrients.
As fluid needs go up, electrolyte needs increase in tandem. Electrolyte deficiencies carry risks, such as issues with fetal growth or certain pregnancy complications.
Since electrolytes essentially dissolve in fluids, it’s important that the concentration of electrolytes is maintained even with higher fluid needs. If your only response to increased hydration is to drink lots of water, but there is no concurrent increase in electrolyte intake, a variety of potential complications can arise. More on this below.
Sodium and chloride (Don’t fear salt during pregnancy!)
Sodium and chloride go hand in hand because they are the two minerals found in salt. Although salt often gets a bad rap, it is vital to the normal function of your body. The sodium and chloride it contains are key for electrolyte balance (to keep your cells talking to one another), helping to maintain the correct plasma volume in your bloodstream (to regulate fluid levels), and facilitating neural signaling (so you can think straight and move your muscles on command).
As I mentioned before, as fluid volume increases during pregnancy, there is likewise an increased need for electrolytes, including salt (this shift begins in the first trimester, by the way!). If you’ve ever gone to the hospital and received IV fluids, you did not receive pure, distilled water. At minimum, you received saline (salt water) because the body requires sodium alongside fluids to rehydrate.
Salt also supports normal stomach acid levels by supplying chloride; stomach acid is hydrochloric acid. Adequate stomach acid is necessary for the absorption of minerals and vitamin B12, for facilitating protein digestion, and for killing off pathogenic bacteria before food leaves your stomach. In addition, salt plays an important role in food preservation, preventing unfriendly organisms from growing in food that could make you sick.
While conventional nutrition frequently touts a low-salt diet to prevent high blood pressure, this is not evidence-based advice. For most people, salt does not have an impact on blood pressure. In fact, only about 25% of the population is salt-sensitive (meaning only a quarter of us will see our blood pressure go up from eating salt). Plus, 15% of the population will have elevated blood pressure on a low-salt diet.
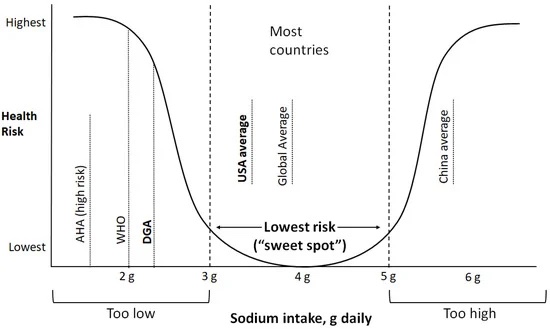
While many nutrition guidelines suggest limiting sodium intake to less than 2,300 mg per day, this recommendation is not supported by robust evidence. A 2021 review on sodium intake across the world found that an intake of 3,000 to 5,000 mg of sodium per day is associated with the lowest risk of adverse health outcomes, including cardiovascular disease. Keep in mind that this study was not looking for optimal sodium intake in pregnancy specifically; that has yet to be defined.
Interestingly, non-pregnant women with low sodium intakes (<1,500 mg per day) have been observed to have significantly lower progesterone levels (37% lower) compared to women who consume enough salt. Given the importance of progesterone to ovulation, conception, and a healthy pregnancy, you’ll want to think twice about restricting your salt intake if you’re pregnant (or trying to conceive!).
What about a low salt diet to prevent preeclampsia?
Despite our prenatal nutrition guidelines suggesting otherwise, the evidence in pregnancy does not support a low-salt diet as a means to prevent or control high blood pressure nor preeclampsia. We’ve known since the 1950s that preeclampsia symptoms could be significantly lessened with higher salt intake (the researchers even use the words “spontaneously resolve”). Furthermore, a low salt diet can have serious consequences on your baby’s development. Low salt intakes during pregnancy have been connected to intrauterine growth restriction or death, low birth weight, organ underdevelopment and dysfunction in adulthood. It has also been found that salt-restriction during critical development periods might affect fetal hormonal, vascular, and renal systems to regulate fluid homeostasis to the fetus. Low salt intake can also predispose you to fluid regulation issues; both volume depletion (low amniotic fluid) and polyhydroaminos (excessive amniotic fluid) have been linked to insufficient maternal sodium levels. And if all of that wasn’t significant enough, research has found that low salt intake can worsen blood sugar and insulin resistance, both of which are undesirable during pregnancy. For more on high blood pressure in pregnancy as well as the research on salt, see chapter 7 of Real Food for Pregnancy. Reducing the risk of preeclampsia or lessening blood pressure goes far beyond this brief conversation about salt.
Maybe hearing all of this makes you want to go grab some potato chips or Cheetos. The takeaway message here is not to eat more processed foods. Americans already eat 58% of their calories from ultra processed food, which is doing us no favors whatsoever. Fully 90% of added sugar intake in the U.S. diet is from these ultra-processed foods. Elevated blood sugar (from eating said ultra-processed foods) is a major contributor to high blood pressure, not to mention all the additives and chemicals used in processed foods. Salt often gets the blame, but that’s nutritionism for you (i.e. try to single out the one dietary villain).
It’s important to consume salt in the context of a real food diet. This way, the sodium is balanced with other complementary nutrients (like potassium) as well as sufficient fluid intake. I recommend switching to unrefined sea salt (I like Redmond’s Real Salt; code LILY to save) to get additional trace elements that you won’t find in kosher or table salt. Let your taste buds be your guide! In fact, some of the most common food cravings during pregnancy — pickles, olives, cheese — are for sodium-rich foods. There’s a good chance that if you’re craving those foods, you may need extra salt in your diet.
Common signs of insufficient sodium intake are: swelling (I know it’s counterintuitive to decades of advice to the contrary, but it’s true), headaches, leg cramps, fatigue, and high blood pressure.
Anyone who sweats a lot, such as athletes or those who live in very hot climates need to be especially careful to increase sodium intake to account for losses in sweat. Also, if you have recently reduced your carbohydrate intake, keep in mind that higher amounts of sodium are excreted in your urine on such a diet (as insulin levels drop, more sodium is excreted). Therefore, low carb eaters need to be especially careful to eat enough salt (this is precisely the reason that the company LMNT was founded).
Sodium-rich foods: While salt is the most concentrated source of sodium, you don’t just have to rely on your salt-shaker to increase your intake. Miso, sun-dried tomatoes (if salt is used in the curing process), pork rinds, bacon, salami, beef jerky, Parmesan cheese, pepperoni, sausage, olives, pickles and other lacto-fermented vegetables, like sauerkraut or kimchi, are concentrated sources of sodium.
Potassium and pregnancy
Bananas, potatoes, avocados… all great sources of potassium that you may have heard nutritionists encourage. But why? Potassium is one of the minerals that balances the effects of sodium in our cells. As sodium increases, potassium intake should increase, too! Potassium works with other minerals to maintain normal fluid electrolyte balance. It is also important for fetal growth, insulin sensitivity, and blood pressure regulation.
Unfortunately, potassium has been understudied in pregnancy. The current potassium intake recommendations are based on needs for nonpregnant females. This is because researchers have not found that potassium accumulates during pregnancy, so they do not anticipate that pregnant women need more of it. The most recently revised recommendation (as of 2017) for both pregnant and non-pregnant women is around 4,000 mg/day of potassium. However, during lactation, an additional 400 mg of potassium is needed to account for what is secreted in breast milk (suggesting an optimal intake of 4,400 mg per day). The meal plans in Real Food for Pregnancy all contain more than 4,000 mg of potassium per day (some are even > 4,700 mg/day!).
Insufficient intake of potassium has been implicated in preeclampsia and high blood pressure during pregnancy. For example, researchers have observed that women with a more balanced ratio of potassium to sodium have lower blood pressure levels, lower frequency of severe preeclampsia, less kidney damage and better perinatal outcomes (preterm birth and low birth weight) than those with an imbalance ratio of the two minerals. An imbalanced intake of sodium to potassium is a hallmark of a diet high in processed foods. This is one reason that it’s key to view sodium intake in context of diet quality!
Potassium-rich foods: While bananas are a well-known potassium-rich food, there are actually many other foods that have equal or higher potassium concentrations. You may be surprised to learn that sun-dried tomatoes, avocado, bacon, ham, salmon, dried apricots, hearts of palm, coconut water, citrus, potatoes, shiitake mushrooms, parmesan cheese, milk, tomato paste, and beans (lima, kidney, black beans) are all foods with high potassium concentrations.
Potassium-rich electrolyte beverage: You’ll see coconut water in the above list of potassium-rich foods. If that’s not available to you, there’s a really delicious electrolyte beverage called Rayvi (founded by a fellow dietitian!) that uses coconut water powder as a primary ingredient. You simply mix it with water and you’ve got yourself over 450 mg of potassium per serving! I sometimes mix Rayvi and a packet of LMNT for a supercharged electrolyte beverage. Check out the Rayvi line of flavors here. They’re fancy like passion pineapple, golden ginger turmeric, and hibiscus mintberry. Rayvi would be a great option to have on hand for labor!
Interesting tidbit on cream of tartar: Some people also increase their potassium intake by adding a little bit of cream of tartar powder to their beverages or electrolyte drinks. Cream of tartar is potassium bitartrate (potassium bound to tartaric acid; tartaric acid is a byproduct of the wine industry, but don’t worry, no alcohol is left in it). One teaspoon of cream of tartar provides 495 mg of potassium.
Magnesium and pregnancy
Magnesium has its hands in almost every metabolic pathway in the human body — really! Magnesium has over 600+ roles in enzymatic reactions in the body, including all the steps involved in Vitamin D metabolism. It also helps with insulin regulation, muscle relaxation, fetal bone formation, and immune function. Plus, it may help alleviate morning sickness in pregnancy. As you can see, you need magnesium for just about everything!
Unfortunately, magnesium deficiency in pregnancy (and for most adults) is common. The soil used to grow our crops is not as magnesium-rich as it used to be thanks to heavy pesticide use on commercial farms. In pregnancy, magnesium deficiency is commonly found in women with gestational diabetes and preeclampsia.
In pregnancy, strive for magnesium intake of no less than 300-500 mg/day (your provider may recommend more). According to recent estimates, 48% of Americans consume inadequate magnesium from food and among women aged 19-30 specifically, 64% do not meet recommended intake levels. These estimates are assuming that the food we’re eating is just as magnesium-rich as it was when the nutrient databases were originally created, so the true statistics are probably much more dismal.
Magnesium supplementation: It can be challenging to reach optimal intakes of magnesium from food alone and this is where supplementation can come in handy. The form of magnesium is important to consider, since some forms can be difficult to absorb. Magnesium glycinate and malate are well-absorbed forms and unlikely to cause any GI upset. Magnesium citrate is another option, however it can result in loose stools if consumed in excess (a good option if you struggle with constipation). Finally, I recommend avoiding magnesium oxide or sulfate as an oral supplement; these are specifically used as strong laxatives. Magnesium sulfate (Epsom salts) can, however, be used in baths or foot soaks (yes, transdermal absorption works). There are also magnesium “oil” lotions and sprays made with magnesium chloride that are also effective for increasing magnesium levels. See below for brand/product recommendations.
If you are suffering from frequent leg or muscle cramps, are at risk for high blood pressure/preeclampsia, or have insulin resistance or gestational diabetes, supplementation of magnesium may be especially helpful. A meta analysis of the trials on magnesium supplementation in pregnancy found that it significantly reduced the risk of preeclampsia (by 24%), particularly in women considered high-risk for this condition.
For a list of recommended magnesium supplements, see my Fullscript recommendations (under the heading “magnesium”). You’re welcome to purchase those supplements anywhere, but purchases made directly through my Fullscript are discounted below retail prices.
One of my favorite magnesium products is the magnesium glycinate powder from Seeking Health. Each scoop has 200 mg of magnesium and it dissolves super well in water and doesn’t have a yucky flavor (unlike so many other forms of magnesium). They also make a magnesium malate powder that can be used in the same way. I often add a scoop of either one to my electrolyte drinks, such as LMNT.
If you’re taking a comprehensive prenatal vitamin (like this one or this one), there may be a good amount of magnesium in it, but most on the market, especially if they’re less than 3-4 pill serving/day have either NONE or only pixie dust amounts (minerals take up a lot of capsule space!). You can also get some magnesium through electrolyte drinks, such as LMNT, which has 60 mg per packet, or Rayvi, which has 45 mg per serving.
Magnesium-rich foods: Magnesium is readily found in pumpkin seeds, flaxseed, brazil nuts, peanuts, sunflower seeds, chia seeds, almonds, tahini, sesame seeds, poppy seeds, leafy greens, culinary herbs, cocoa, and seaweed. (Keep in mind that for greens and culinary herbs, the serving size needed to provide much magnesium is quite large.) Magnesium is also concentrated in some types of seafood, such as caviar (fish eggs), cod, salmon, and halibut.
Calcium and pregnancy
Calcium is an interesting electrolyte because while it has major contributions to fetal growth, calcium needs do not increase during pregnancy. The absorption of calcium actually doubles during pregnancy meaning you will take in more of the calcium from what you’re already eating. Calcium is responsible for bone development, muscle and nerve function, and enzyme and hormone activity. Because these functions are so important it seems to me like the body is doing us a favor – it knows it needs more calcium for the growing baby so it works overtime for us!
The RDA for calcium during pregnancy is 1,000 mg/day. The Standard American Diet typically provides an average of 838 mg/day – pretty close to the RDA. However, our diets are often lacking in other major nutrients that are critical for calcium uptake and absorption; Vitamin D, vitamin K2, and magnesium are all needed to process calcium. You’ll find more of these nutrients in a real food meal plan like the ones I provide in Real Food for Pregnancy. Plus, my meal plans will meet recommended intakes, providing on average, >1200 mg/day of calcium.
Since most women will be able to meet their calcium needs through food, supplementation of calcium during pregnancy is not commonly necessary. However, for women with preeclampsia, some studies suggest that supplementing with 500 mg/day of calcium can help alleviate high blood pressure in pregnancy and may reduce related complications. Calcium in the form of calcium malate or egg shell-derived calcium are better absorbed and utilized by the body (avoid calcium carbonate, which is literally ground up chalk).
Calcium-rich foods: The most concentrated sources of calcium are in cheese and milk products, so those who are dairy-free* will need to be extra intentional about finding calcium-rich non-dairy sources (especially vegans). Adequate intakes of calcium can be met on a dairy-free diet with inclusion of calcium-rich foods such as sesame seeds, chia seeds, tahini, and fish that are canned with the bones (such as salmon canned with the bones, or sardines canned with the bones).
*If you’re dairy-free, keep in mind that dairy products provide many of the complementary nutrients that support calcium absorption (such as vitamin K2 and D), so you’ll also need to be more intentional about obtaining enough of these nutrients. A high quality prenatal vitamin, such as FullWell (code LILY10 to save) or Seeking Health, is especially important if this is you. These nutrients help direct calcium to where they are needed most — bones and teeth — so they don’t accumulate in the wrong places, like blood vessels, soft tissues, or the placenta.
Tips for increasing electrolytes during pregnancy
As you can see, consuming adequate electrolytes during pregnancy is important for you and your baby’s health. Here are a few strategies for increasing your electrolytes:
- Eat real, whole foods, preferably sourced from local farms with high quality soil. A diet that includes both plant and animal foods makes it easiest to meet electrolyte requirements.
- Liberally season your whole foods with salt to taste – you’ll get more sodium and chloride (and I bet those vegetables will taste better). If you crave salty foods, there’s a good chance your body can benefit from more sodium.
- Focus on including potassium-rich foods in your diet (there are plenty of options beyond bananas and potatoes if those don’t appeal to you). Coconut water, Rayvi, or even a pinch of cream of tartar in your water can boost intake.
- Try a homemade electrolyte drink. Find a recipe for one in Real Food for Pregnancy or create your own using LMNT packets or Rayvi. LMNT is a blend of sodium, potassium, and magnesium. You can get a free sample pack of LMNT with purchase using this link. I especially like the orange, watermelon, or grapefruit flavors dissolved in ~24-32 ounces of water, plus a squeeze of lemon, lime or grapefruit. In the winter, I like the chocolate or chocolate mint flavor as a hot cocoa (dissolve in hot water and add a splash of cream/milk). If LMNT is too salty for you, try Rayvi, which is a high-potassium electrolyte drink mix featuring coconut water powder as a primary ingredient that comes in several gourmet flavors.
- In addition to prioritizing magnesium-rich foods, consider taking a magnesium supplement. See above for preferred forms.
Summary
Electrolytes have so many important functions during pregnancy that it is a good idea to focus on increasing your intake of these as best you can.
- Electrolytes are essential minerals that carry an electric charge once dissolved in fluid. Sodium, potassium, chloride, calcium, and magnesium all act as electrolytes.
- Electrolytes are necessary for keeping your heart beating normally, keeping fluids in balance, supporting adrenal health, and for alleviating common annoyances like headaches, muscle cramps, and swelling.
- As fluid needs increase during pregnancy, electrolyte needs also increase to maintain a good balance of electrolytes to fluids.
- Salt contains both sodium and chloride which are key for electrolyte balance, regulating fluid balance, and facilitating neural signaling.
- Potassium works with other minerals to maintain normal fluid electrolyte balance and is important for fetal growth, insulin sensitivity, and blood pressure regulation.
- Magnesium plays a role in over 600 reactions in the body and plays a key role in blood sugar and blood pressure regulation. This is a tricky one to get solely from food, so a supplement is often a good idea.
- Calcium needs do not increase during pregnancy but our body’s ability to absorb calcium doubles. Most of us can meet calcium requirements from food alone, but there can be exceptions.
- You can increase your electrolyte intake by eating real, whole foods sourced from locally grown farms with good soil integrity that are seasoned liberally with salt. You can also consider an electrolyte supplement/beverage (see above tips for increasing electrolyte intake).
Until next time,
Lily
PS – If you’ve noticed a benefit in adding more electrolytes during pregnancy, let me know in the comments below.
References
- Terry, Judy. “The major electrolytes: sodium, potassium, and chloride.” Journal of intravenous nursing: the official publication of the Intravenous Nurses Society 17.5 (1994): 240-247.; Terry, Judy. “The other electrolytes: magnesium, calcium, and phosphorus.” Journal of intravenous nursing: the official publication of the Intravenous Nurses Society 14.3 (1991): 167-176.
- Ingram, M, and AG Kitchell. “Salt as a preservative for foods.” International Journal of Food Science & Technology 2.1 (1967): 1-15.
- Gildea, John J et al. “A linear relationship between the ex-vivo sodium mediated expression of two sodium regulatory pathways as a surrogate marker of salt sensitivity of blood pressure in exfoliated human renal proximal tubule cells: the virtual renal biopsy.” Clinica Chimica Acta 421 (2013): 236-242.
- Mente, Andrew, et al. “Sodium Intake and Health: What Should We Recommend Based on the Current Evidence?.” Nutrients 13.9 (2021): 3232.
- Kim, Keewan, et al. “Dietary minerals, reproductive hormone levels and sporadic anovulation: associations in healthy women with regular menstrual cycles.” British Journal of Nutrition 120.1 (2018): 81-89.
- Sakuyama, Hiroe, et al. “Influence of gestational salt restriction in fetal growth and in development of diseases in adulthood.” Journal of biomedical science 23.1 (2016): 1-9.
- Guan, J., et al. “Fetal development of regulatory mechanisms for body fluid homeostasis.” Brazilian Journal of Medical and Biological Research 41.6 (2008): 446-454.
- arta, Valerie, and Holly Koncicki. “Electrolyte disorders in pregnancy.” Obstetric and Gynecologic Nephrology. Springer, Cham, 2020. 113-127.
- Iwaoka, T., et al. “The effect of low and high NaCl diets on oral glucose tolerance.” Klinische Wochenschrift 66.16 (1988): 724-728.
- Strohm, Daniela, et al. “Revised reference values for potassium intake.” Annals of Nutrition and Metabolism 71.1-2 (2017): 118-124.
- Yılmaz, Zehra Vural et al. “Dietary sodium and potassium intake were associated with hypertension, kidney damage and adverse perinatal outcome in pregnant women with preeclampsia”. Hypertension in Pregnancy 36.1 (2016): 77-83. Online. Internet. 15 May 2022.
- Guo, Wanli, et al. “Magnesium deficiency in plants: An urgent problem.” The Crop Journal 4.2 (2016): 83-91.
- Mäder, Paul, et al. “Soil fertility and biodiversity in organic farming.” Science 296.5573 (2002): 1694-1697.
- Bardicef, Mordechai, et al. “Extracellular and intracellular magnesium depletion in pregnancy and gestational diabetes.” American journal of obstetrics and gynecology 172.3 (1995): 1009-1013.
- Rosanoff, Andrea, et al. “Suboptimal magnesium status in the United States: are the health consequences underestimated?.” Nutrition Reviews 70.3 (2012): 153-164.
- Dahle, Lars O., et al. “The effect of oral magnesium substitution on pregnancy-induced leg cramps.” American journal of obstetrics and gynecology 173.1 (1995): 175-180.
- Rylander, Ragnar, and Maria Bullarbo. “[304-POS]: Use of oral magnesium to prevent gestational hypertension.” Pregnancy Hypertension: An International Journal of Women’s Cardiovascular Health 5.1 (2015): 150.
- Yuan, Jing, et al. “Oral Magnesium Supplementation for the Prevention of Preeclampsia: A Meta-analysis of Randomized Controlled Trials.” Biological Trace Element Research (2021): 1-10.
- Kovacs, Christopher S. “Maternal mineral and bone metabolism during pregnancy, lactation, and post-weaning recovery.” Physiological reviews 96.2 (2016): 449-547.
- Bailey, Regan L., et al. “Estimation of total usual calcium and vitamin D intakes in the United States.” The Journal of nutrition 140.4 (2010): 817-822.
- Hofmeyr, G. J. “Prevention of pre-eclampsia: calcium supplementation and other strategies.” Obstetrics and Gynaecology Forum. Vol. 26. No. 3. In House Publications, 2016.



I take LMNT daily and use a small amount of topical magnesium lotion before bed. I’m in my third trimester getting the best sleep of my life and absolutely ZERO swelling
Hooray!!!
May I ask what topic magnesium lotion you use? 🙂
Great article! I had been having a lot of issues with sleep a few months ago and thought it might be an electrolyte issue. I started adding electrolyte drops and Redmond salt to my water and taking magnesium threonate in the middle of the day (interestingly taking it just before bed didn’t work but earlier in the day did) and immediately started sleeping so much better! Wasn’t waking up constantly throughout the night anymore.
Would love to hear your thoughts on electolyte needs for women who remain active during their pregnancies. Are they greatly increased or not as much as we’d imagine?
It depends on how much you sweat. More sweat = more electrolyte losses.
Are electrolytes essential during breastfeeding as well? Is it ok to consume an lmnt packet daily? How would you know if you’re getting too many electrolytes?
Yes, key to consume enough electrolytes during breastfeeding since electrolytes are transferred via breastmilk. It’s hard to get too many electrolytes. Your body simply filters out any excess and excretes it in your urine/stool. That said, if you’re having loose bowel movements, it may be too many electrolytes for you (or in one sitting), so that can be a sign to taper back a bit.
How do you know if you’re getting too much salt? How many relyte packets a day while pregnant or breastfeeding if eating a Whole Foods diet (in your opinion ) ?
Great article as always! I was wondering what does research say about electrolytes postpartum? Specifically for breastfeeding.
Came here to ask this, too!
Electrolyte needs are even higher during breastfeeding since electrolytes are transferred via breastmilk. Whatever you’re doing during pregnancy, continue plus some!
I’ve had GD with both pregnancies. First time I definitely didn’t drink enough water and did not intentionally add electrolytes. I woke up with a leg cramp every night for the last 5 wks or so!
Fwd to second pregnancy. I increased my water intake and after a leg cramp one night i decided to add a nightly electrolyte drink. I had just that one leg cramp the entire pregnancy.
The addition of electrolytes dramatically improved my experience.
Do it!
(I used Key Nutrients if you want to check those out)
Amazing testament to the value of electrolytes in pregnancy. Those leg cramps can be brutal!
I started drinking One or two Liquid IV, Kinderlyte, or LMNT a day in my second trimester and have noticed significant differences. I’m sleeping better, releasing stress, and having fewer muscle cramps. Honestly,I feel happier too! Liquid Iv and Kinderlyte were too sweet, I’m sticking with LMNT..
Love this! Just found out I’m pregnant and I’ve been taking LMNT everyday and was just about to research if I should continue this during pregnancy. Thanks Lily for another amazing blog and research!
Such a great article, thank you! I added pink sea salt to taste throughout pregnancy, plus magnesium glycinate, and never suffered from any swelling, cramps (maybe once or twice only!), and adding some salt w/ bone broth was always the cure for any headache or fatigue too. Adding more salt to my diet also significantly reduced any fast food cravings – which makes sense. Big benefit for my health! I also recovered rapidly from labor (with having lost 1L of blood) with using coconut water & salt to taste. They always tell you to drink more water, but don’t mention you need a pinch of salt with each bottle in order to retain those fluids for you and your baby. Thanks Lily for this excellent advice. xx
Appreciate hearing your experience on the benefits of electrolytes during pregnancy (and for postpartum recovery)!
I have a milk protein allergy, and I was wondering if you had any further tips on getting enough vitamin K2 through real food? I have tried ghee but I am still sensitive to it, so wondering what else I can try. Do you think synthetic Vit D/K2 sprays are good, or not? I’ve heard that they are fat-soluble so should be taken only as cod liver oil, etc? Thank you 🙂
I’m currently in my third trimester and noticed that when drank a half packet of LMNT a day I started getting a lot of heart palpitations after the drink so I stopped it and the heart palpitations stopped. Not sure what the reason might be, would you happen to have any insight on that? Would love to continue drinking electrolytes because there was a noticeable difference in my hydration levels , but worries about the palpitations.
I experienced heart palpitations for the first time when I started taking cream of tartar to increase my potassium intake. I was taking less than a teaspoon, but apparently that was too much for my body, and after I quit taking cream of tartar the palpitations stopped.
I later found out that high potassium levels in the blood can cause palpitations (as can low electrolyte levels). This isn’t a concern with potassium from food because digestion slows the absorption, but with potassium supplements, taking too much at a time can be dangerous because it raises the blood levels so quickly (which is why potassium supplements tend to only provide 99 mg or less).
It needs to be taken in an appropriate balance to other electrolytes. This is why any homemade electrolyte drinks that contain cream of tartar also contain sufficient sodium. It should not be taken alone.
Are you supportive of stevia and monk fruit use in pregnancy?
Have you looked into the safety of these ingredients in pregnancy? Both electrolytes products you promote use at least one of these ingredients.
Yes, neither raise safety concerns when used in moderation. The research on stevia is addressed in Ch 4 of Real Food for Pregnancy.
Supplementing electrolytes in pregnancy completely curbed my morning sickness. I would love to see that studied!
I hear this often and personally experienced the same. I especially needed more salt to ease my nausea.
Great article! As a nurse practitioner in an OBGYN office I am CONSTANTLY promoting electrolyte replacements with my patients. I always tell them that they can be dehydrated even when getting enough water. Thanks for all the good information I can pass along to my patients.
Thank you for educating your clients on the importance of electrolytes during pregnancy!
Thank you for always being my informative go-to during my pregnancy, Lily. You rock! I keep coming back to your book for info, but now I’d love to share it.
Is Real Food for Pregnancy available in French? If so please could you let me know how I could get this in Switzerland?
Thank you in advance!
Thanks so much! It’s not yet available in French. Hopefully sometime soon!
Thank you so much for this article! I just discovered your work on a podcast I listen to and have been binge-reading your blog and book ever since! Thanks for your evidence-based insights and I really appreciate your non-alarmist way of communicating. Keep up the great work!
After 3 pregnancies and no active management of my electrolytes I suddenly developed terrible ocular migraines on about a weekly basis, really impacted my ability to work . Countless specialist visits later and literally every dr stumped, I ordered a supply of LMNT. Migraines completely disappeared and come back again as soon as I miss a few days. LMNT has been a game changer for me… only wish I had figured it out sooner. Curious if anyone else has had this experience?
Wow, so glad you’ve figured that out. I frequently see electrolyte insufficiency playing a major role in headaches/migraines.
I had developed pretty consistent migraines during this pregnancy (only occasional prior to conception). My midwife recommended the Liquid IV that has green tea in it. My migraines went away once I started using those and headaches only come back if I miss some kind of electrolyte supplement. I have had consistent results with the regular liquid IV and Hilyte as well 🙂
Is there any research on Stevia during pregnancy? I know all but the unflavored LMNT have Stevia. Thanks!
Hi Lily, just wondering if you have come across any information on oligohydraminos (low amniotic fluid) and electrolytes. I have had oligo on two pregnancies although I made a conscious effort to drink more water in the second pregnancy. Thank you for all your work
At what time would be the best to drink electrolytes, before going to bed? Lately I been waking up about 4 times during the night and feel very tired in the morning
Hi! It sounds like you maintain a list of recommended supplements on Fullscript, but the link you included (https://us.fullscript.com/welcome/lilynichols) redirects first to a login page, and then after login, to a generic catalog page (https://us.fullscript.com/u/catalog). Can you provide another link to your recommendations?
After you log in to Fullscript, click the recommendation tab at the top > Shared Protocols. Hope this helps!
I’m wondering if trace mineral drops added to water cover most of the needs for electrolytes?
Magnesium has been a lifesaver for me these past 20 weeks! I had restless legs starting right at the beginning of my pregnancy. I take a magnesium supplement right before bed, and I have been having the best sleeps of my life.
Hi Lily!
I have started taking the magnesium glyconate you recommended before bed to help with sleeping. When I mix it with my beverage it turns green. Is this safe? Does this cancel out the affects of the magnesium?