Last week, I left you hanging about the results of my glucola.
One of my readers emailed me:
“Damn cliff hanger!! I want to know your results. Lol. This is why I binge watch tv shows after the whole season is out. The suspense is killing me.”
Who knew a glucose tolerance test could be described as “suspenseful?!” (other than me, of course…)
I was certainly curious to get the results of my test. When the lab technician said they could run the analysis in office, I decided to stick around for a few extra minutes. (Plus, I just had to finish the riveting article I was reading in Alaska Sporting Magazine…)
I was sure I had passed, so when the lab tech said:
“You should have studied better.”
I knew he was joking.
But he wasn’t.
I got a 141.
Passing is <140.
I was kind of shocked.
I failed the glucola. Now what?
Now, the 1-hour, 50 gram glucola is NOT diagnostic of gestational diabetes on its own. It is a screening test to identify those at “high risk” and determine who should get further testing.
He said my next step was to come back again for the 3-hour test. Of course, since I specialize in gestational diabetes, I knew all that.
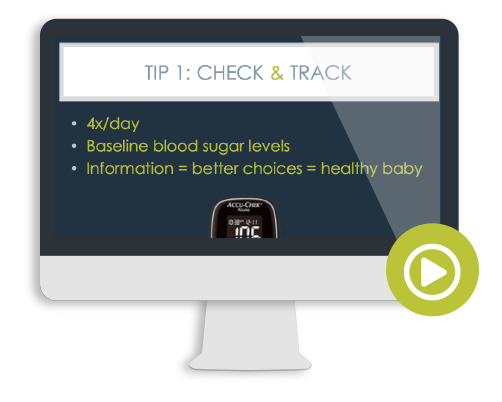
I had already discussed testing options with my doctor and had decided that regardless of the results of the 1-hour, 50g screening that I would check my blood sugar at home with a glucometer for 2 weeks just for my own knowledge. In fact, I already had my prescription for blood sugar testing supplies in hand before I drank the glucola.
Still, I walked out of the office feeling like a failure.
How could I not feel that way? The official medical terminology is “passing” or “failing.”
I cursed under my breath as I made my way to the car.
A million thoughts raced through my head:
- Should I have opted out of the dumb test and just done home glucose monitoring?
- Now are they going to pressure me into doing the 3-hour test (with double the sugar)?
- What if I really do have gestational diabetes? I know how to manage it, but would my birthing options be limited? Would I be treated differently by my doctor?
- Why didn’t I carb-load for the past week?! I knew my moderately low-carb, low-glycemic diet made it more likely for me to get a false positive. I’m such an idiot.
- I shouldn’t have skipped my walk this morning. If I had exercised, like usual, I would have had better insulin sensitivity. Maybe I should have done squats in the bathroom?!
And then the other part of me was thinking…
- If you had carb-loaded for a week, technically you would have been “cheating the test.” Yes, you likely would have passed, but YOU were the one who wanted to see the results based on what you usually eat and here you have ‘em. You confirmed what’s been well-documented in the literature for decades. (See NEJM, 1960)
- If you had exercised immediately before – or during – the test, yes, you may have gotten a lower reading… But there are days when you don’t walk or exercise, and now I know how my blood sugar would respond on those days IF I ate 50g of pure sugar. (I’m sure as hell glad I DON’T eat 50g of sugar, pretty much EVER. Now I know how my body responds to it.)
- Your first trimester A1c was low, so you definitely didn’t have prediabetes, and your weight gain is within normal, so the likelihood that you have GD is still pretty slim.
- Numbers are simply information, not “good” or “bad.” Just like you tell your clients, you need to test at home and see where your blood sugar is at before you choose your next steps.
- Of all people, you know what to do. No matter what you find out from testing your blood sugar at home, you’ll be able to manage it.
I’m usually a pretty rational person, but my mind was all over the place.
Maybe my erratic blood sugar was clouding my judgement.
By the time I had picked up my blood sugar testing supplies and got home, I felt like I was having reactive hypoglycemia. Hungry, moody, a little shaky… It had been a long time since I felt that.
So the first thing I did when I got home was wash my hands and test my blood sugar.
I got a 129.
This was now 2 hours after I drank the glucola.
“Holy shit. I really DO have gestational diabetes! I’m insanely insulin resistant.”
So I got myself a low-carb snack (figuring I didn’t want to spike my blood sugar any higher), then dinner a few hours later, and anxiously anticipated my blood sugar reading after my meal.
It was 87.
100% normal.
Granted, that meal was real food – not 50g of sugar – but I still didn’t understand why my insulin response 2 hours after the glucola was so dismal. Plus, I was hungry at that time. If you’re hungry, it’s usually a good sign your blood sugar is on the lower end, especially if you have normal insulin sensitivity.
My pancreas must suck.
I was stumped.
And then I got thinking… I had recently refilled my hand soap at the kitchen sink. That’s what I washed my hands with when I tested my blood sugar the first time. After dinner, I washed my hands in the bathroom with different soap.
I hunted down the original bottle for the Burt’s Bees liquid soap I had used to refill the kitchen hand soap.
And let me tell you, I laughed as I read the ingredients. Among them were eight – yes EIGHT – sugar-derived ingredients (such as lauryl glucoside, sucrose laurate, and even straight-up GLUCOSE).
You’d think as a certified diabetes educator, I’d know better. Hell, I DO!
I’m just glad I realized on day 1 of testing NOT to use that soap before checking my blood sugar!
So that reading of 129 was really just telling me that my hands were covered in sugar. Great.
(I should have thought to wash my hands again and re-test, but in my post-glucola stupor, that didn’t even cross my mind.)
I knew I needed more data. A few blood sugar readings don’t reveal much.
To see if I truly had gestational diabetes or not, I would need at least 1 week’s worth of blood sugar readings (preferably more, in my opinion).
I was very curious to check my fasting blood sugar – the reading taken first thing in the morning – because that often gives a sneak peek into your baseline blood sugar levels.
The next morning I got a 73.
In all my years working with women with gestational diabetes, I’ve had one GD client who had fasting blood sugars in the 70’s. Myself and the perinatologist agreed she had been misdiagnosed (she, like me, had eaten a low-carb diet prior to her GTT).
Nonetheless – and for the sake of science – I have continued to test my blood sugar (nearing 2 weeks now) – both fasting and after meals – to see where I’m at.
Eating my usual, real food diet has given me perfectly normal blood sugar readings.
I’ve also purposefully had some high-carb meals to see my tolerance to a similar amount of carbohydrate as the glucola, but in the form of a mixed meal.
My doctor had requested post-meal blood sugar #s be taken 2-hours after meals, but I’ve checked at both 1 and 2 hours out of curiosity for some meals (some women spike at 1 hour, others at 2 hours, so I wanted a more complete picture of what was going on in my body).
The highest carbohydrate meal I tried was 50g total carbs (45g net carbs): gluten-free butternut squash ravioli (intentionally overcooked to further raise the glycemic index) with sausage, kale, mushrooms, and butter.
My results?
1 hour later: 114
2 hours later: 86
This was a larger portion than I normally serve myself and I was full before I cleared my plate, but since I had already calculated out the nutrient content, I wanted to finish it… again, for science!
I repeated the same meal a few days later with similar results:
1 hour later: 104
2 hours later: 89
My usual meals vary in carb content, but I rarely reach 45g carbs per meal, so it was reassuring to get “normal” readings.
(In case you’re wondering, I have been tracking my macronutrients during this time. I know from experience that most people, myself included, underestimate how many carbohydrates they eat – sometimes by quite a bit! So I wanted to have a more accurate idea of where I fall on the carb spectrum. While it’s been helpful for the purpose of collecting data, I fully recognize the downsides of tracking macronutrients and will be quitting at the end of this experiment. It really does make it challenging to remain a mindful eater with all these numbers getting in the way!)
I’m nearing the end of the 2-week experiment and have not had a single reading out of range.
My post-meal readings have only gone beyond 100 a few times – all from high-carbohydrate meals. (The 114 I mentioned above was, by far, my highest reading.)
My fasting blood sugar numbers remained steady as well (and I didn’t employ the advanced tips & tricks for naturally lowering fasting blood sugar that I teach in the Real Food for Gestational Diabetes Course).
My average fasting blood sugar is 75.
My average blood sugar after meals is 87.
For those of you familiar with conventional gestational diabetes target blood sugar levels (or especially non-pregnancy blood sugar targets), you might think my readings are too low.
I assure you, they are not.
As covered in my book, Real Food for Gestational Diabetes, average blood sugar levels in healthy pregnant women are as follows: (Diabetes Care, 2011)
- Fasting: 70.9 +/- 7.8mg/dl
- 1 hour post-meal: 108.9 +/- 12.9mg/dl
- 2 hours post-meal: 99.3 +/- 10.2mg/dl
It’s safe to say, I do not have gestational diabetes.
But with or without the official diagnosis, I would not eat any differently.
One side benefit of eating a nutrient-dense, real food diet is maintaining normal blood sugar numbers. And given that even mildly elevated blood sugar in pregnancy (below diagnostic thresholds for GD) has been linked to health problems in baby, including the risk of congenital heart defects, I have no intention to eat more refined carbohydrates just because I can “get away with it.” (JAMA Pediatrics, 2015)
The way I eat is delicious, full of nutrition for me and baby, keeps me satisfied, and has helped me stay pretty much craving-free. It’s also kept my weight gain, blood sugar, blood pressure, iron levels (and more) completely normal.
But this experience has reminded me how important it is for our screening methods for gestational diabetes to improve.
If you’re going to bother with drinking the glucola, you’d hope that the results are accurate!
It’s certainly weird to go from working alongside one of the world’s top gestational diabetes perinatologists whose passion is evidence-based care (and in an office that trains UCLA’s medical residents) to a teeny office with family practice doctors who only do prenatal care part-time.
Sadly, routine care is not necessarily evidence-based.
The two-step screening method for gestational diabetes is outdated (that’s the 1-hour, 50g screening followed by the 3-hour, 100g glucose tolerance test). A fairly high percentage of healthy women “fail” the first test while some women with excessive insulin production “pass” it and are never formally diagnosed. For those who go on to take the 3-hour test, diagnosis is delayed for weeks when awaiting the results of the second test. Finally, diagnostic criteria (the cut-off of what’s “normal”) arbitrarily varies doctor-to-doctor.
That’s why the International Association of Diabetes and Pregnancy Study Group (IADPSG), the World Health Organization (WHO), and nearly all countries aside from the United States recommend the more reliable and specific 2-hour, 75g glucose tolerance test, which is done fasting and includes more rigid cut-offs for diagnosis.
This method more accurately identifies women at risk for “adverse pregnancy outcomes” associated with gestational diabetes. (Journal of Perinatology, 2014) Plus, it’s just one test. The primary opposition to it is that, due to stringent diagnostic thresholds, more women would be diagnosed with GD and that may increase healthcare costs. (Though I argue, with low-cost interventions like my real food approach and the long-term health benefits to both mom and baby, these would be negligible or may even result in cost savings.)
I would have rather done that test, but that’s not protocol in my doctor’s office.
(Sidenote: To say that I know more about gestational diabetes than my doctor is the understatement of the century.)
In an ideal world, this glucose tolerance test would also measure insulin levels, as I discussed in my interview with Robb Wolf.
In lieu of a glucose tolerance test, the following are options:
1) A fasting blood sugar (venous blood sample, not a fingerstick), can accurately screen for GD. (Int J Endocrin Metab, 2007) However, it can leave some women undiagnosed – those who have normal fasting levels, but have an impaired post-meal insulin response.
2) First trimester hemoglobin A1c is highly predictive of gestational diabetes, so much so that the California Diabetes and Pregnancy Program: Sweet Success recommends it as a way to diagnose GD (and therefore many women would not need to undergo a glucose tolerance test at all). However, if you do, you’d have a pretty good chance of guessing your results. If your A1c is 5.9% or greater in the first trimester, your chances of “failing” the glucose tolerance test are 98.4%. (Diabetes Care, 2014) But keep in mind, it is NOT an accurate option for screening later in pregnancy, as I discussed in this interview.
3) Home blood sugar monitoring remains the most controversial way to diagnose gestational diabetes. Even though I opted for this option (in addition to first trimester A1c + the 1-hour glucola) and I believe it’s a great one for low-risk women who eat a lower-carbohydrate diet, it has some major drawbacks.
a) For one, it’s time consuming. You need to really be motivated to keep up with checking your blood sugar 4x per day. It’s annoying to set alarms, to carry testing supplies with you, to track what you’re eating, and poke your finger so often. I personally felt the annoyance was worth it and provided more useful, real-life information to me, but for others, it’s easier to just drink the glucola and move on.
b) Your diet impacts the results. This is both a good thing and a bad thing. You get a clear idea of how food affects your blood sugar, but I’ve had women who will purposefully starve themselves or temporarily switch to a very low-carb diet to “pass” the test, then go back to their usual diet that includes oatmeal/cereal for breakfast, fruit smoothies, and large portions of starchy foods or sweets. So, unless you continue to eat the way you normally do, you’re only hurting yourself and your baby.
c) Some women cheat. I’ve had women test other people’s blood sugar (like their husband), just so they can avoid the diagnosis. (When you work in this field long enough, you see just about everything!) Of course, if the diet for managing gestational diabetes actually worked (meaning prevented most women from requiring medication) and tasted good, I think this would be less of an issue… (hence why my real food approach is now being taught in at least one medical school and is being employed in several research studies).
d) The criteria for how many out-of-range blood sugar readings (or how high those #s need to be) to trigger a positive diagnosis is wishy-washy at best. In my situation, all of my numbers were well-below the goal range, so it was pretty cut and dry. But for many women, blood sugar readings hover in the grey zone. In that case, it’s unclear what to do. Personally, if I had questionable numbers, I would continue home blood sugar monitoring as if I had gestational diabetes, but for others that’s just too much work and they want a definitive diagnosis.
How do I feel about my decision to drink the glucola?
At the end of this experiment, I’m glad I drank the glucola. I learned that drinking a bunch of pure sugar spikes my blood sugar more than I’d expect (and been reminded that it makes me feel like crap). I’m also glad I didn’t carb-load just to “cheat the test.” By monitoring my blood sugar at home, I’ve confirmed that the way I eat is indeed right for my body.
Given my response, I probably wouldn’t opt for a glucose tolerance test in the future (unless it also included measurements of my insulin response – for science!), but the experiment – at this point in time – was worth it.
Knowing that blood sugar & insulin levels can shift week-to-week (especially in the 3rd trimester), I will continue checking my blood sugar at home – maybe not after every meal, but occasionally so I can be proactive if my numbers start going up.
Going through this has helped me feel, first-hand, the panic that hits my clients when they “fail” the glucola. I’m just glad I can offer them the support they need to make sense of all the information and get a game plan to manage this with as much ease as possible – both for my private clients and members of the Real Food for Gestational Diabetes Course.
—
Now I’d love to hear from you:
What are your thoughts on the way gestational diabetes is diagnosed?
Did you fail the glucola, like me? Did you go through the same “Do I have gestational diabetes” panic?
If you were officially diagnosed with gestational diabetes, how do you feel about it now?
Tell me in the comments below.
Until next week,
Lily



Hi Lily,
Wow, the power of a label! I don’t know to what extent your treatment options will change, but not much might change for you because you are already living out the most effective treatment (diet). One way or another, you will come up with the right tools and information to continue to advocate for you and your child. Your clients are very fortunate to have you working with them.
Appreciate your kind words, Renata. However, you might want to carefully re-read the post. The 1-hour test is not diagnostic on its own. I opted for home blood sugar monitoring for 2 weeks in lieu of the 3-hour test.
I know this is old but I think it’s absolutely insane that a serious healthcare professional could ever recommend skipping an OGTT with a straight face after failing the one hour screen. other methods aren’t standardized for a reason. The A1C test is bogus for diagnosing this. I’m the perfect example – an A1C of 4.6 at 10 weeks pregnant and I was diagnosed with GD at 27 weeks. My one hour screen was in the 170s. I gained 8 pounds only to that point. A1C means almost nothing in this context except assuring me I didn’t have pregestational diabetes. My A1C throughout my pregnancy never went higher than 4.8 but I definitely had to watch the carbs. I always recommend your book to people but I’m really dismayed to see this post, which basically perpetuates the stigma that only overweight people need to take GD screens seriously.
I actively encourage ALL women to get tested for gestational diabetes – that may be via a glucola/OGTT or it may not be. As explained in this post, an OGTT is not 100% accurate in all cases, particularly if a person is eating a low-carbohydrate diet. This is why other methods of testing are options.
For example, in clients who cannot tolerate an OGTT (such as after bariatric surgery or with hyperemesis gravidarum), and in-office fasting blood sugar (venous sample) combined with home blood sugar monitoring are used. As a certified diabetes educator who specializes in gestational diabetes, I can assure you that an OGTT is not the “only” method for diagnosing gestational diabetes.
A detailed and evidence-based discussion of all the screening options for gestational diabetes, can be found in Real Food for Pregnancy.
Wow, Lily. What an incredibly valuable experience. I personally think you made a good decision to do the test because the results (and our reactions) teach us so much about ourselves. Thank you for leading by example. Keep spreading the real food word.
It’s certainly been interesting, Briggite! Thanks for your support and following along. 🙂
This was super helpful! I’m about to go in for my glucola test and I’m nervous about it. This pregnancy I’ve been craving more sugar than usual (even though I’m having a boy) so I’ve had to be very careful with how I eat. Before pregnancy, I ate a lot less sugar. Time will tell but now I know to watch my hand soap and do my own research. Thanks!
Glad it was helpful for you, Kimberly! You can read about my experience drinking the glucola & why I decided to go for it here. 🙂
Oh my god – thank you for writing this post! I, too, just failed the first glucose tolerance test and wonder if I really have gestational diabetes. My test result was borderline (143) and I eat a pretty clean diet without a ton of starchy foods and very rarely eat sweets.
I really don’t feel comfortable doing a second glucose tolerance test with a whopping 100g of sugar. That just seems crazy to me. I don’t want to expose my baby to super high amounts of sugar if I already know my blood sugar was high from half the amount.
I’m going to talk to my doctor about getting a meter. I don’t mind testing my blood sugar for the rest of the pregnancy if that’s what he suggests. I’d rather know where I’m at and manage it than worry. I’m also going to check out your online gestational diabetes course. Sounds like something that would help me out a lot!!!
Hope this gives you some extra info to discuss with your doctor when you make your decision, Lucy.
Interesting read! I failed the one hour at 140 and got talked into the three hour. Had I gone with testing at home, I never would have been diagnosed, or “labeled.”
Like you, I had all those thoughts running through my head.
I’m also really fascinated by your comment that you’ve only seen one person diagnosed with a fasting of 73. I only had fastings between 68-75, typically just at 70 every day of my third trimester. I rarely had a two hour blood sugar above 95. I of course questioned the diagnosis, which my doc didn’t appreciate — it made for a terrible third trimester — and made me resent every single office visit. She told me it was “not uncommon” to see non-GD numbers in a “GD patient,” which makes your comment very interesting!
That’s probably thanks in large part to the way in which we diagnosed gestational diabetes at that office (75g GTT described above), which is more accurate than the 2-step method currently used in the States.
Regardless of an official diagnosis or not, maintaining normal blood sugar is the ultimate goal, so you did a great job. But I’m sorry to hear it caused you so much stress. :/
I have read in several places that a low carb diet often causes women to be more sensitive to the gtt and so that is why some women carb up prior to the test. Why do you consider that cheating when it sounds as if the gtt just is not an accurate way for women on low carb diets to test their blood sugar?
I personally wanted to see how my body responded to the GTT with my usual diet (moderately low carb), not tweak what I was eating just to “pass” the test. Like I explain in the post, this was as much for my own n=1 research than for anything. You can read all the reasons why I agreed to take the (imperfect) test in the first place in this post.
Hi, Lily-
I am checking my blood sugar at home. What do you think about fasting levels between 80-91 and two hour postprandial levels 80-98? I know that the fasting levels are slightly higher than your healthy recommendations above but the postprandial levels are lower than the same recommendations. Thanks!
I’m from New Zealand. We do the 75gm 2hour gtt test here. I remember feeling so sick from the drink. I only just managed to hold out for the two hours and have my blood taken, then vomited my entire stomach contents as soon as I got home. I was confused because I wondered how much I had actually absorbed given that it seemed to all come out again! Sorry I know that’s unpleasant.
My results were borderline so I started testing my blood sugars at home and I developed GD within a few weeks. I initially tried to go paleo and not eat starch to try control my levels. But the dietician told me I needed to eat carbs. 15 grams were the unit of measurement and I needed 10 to 12 units per day as a pregnant woman. I ended up needing insulin and though overall things went well I had a week of failed inductions, an emergency c-section delivery and then my baby had a week in NICU (for suspected infection, but his blood sugar levels were fine).
So now I’m at the beginning of pregnancy #2 and I want to see if I can do things better. My boy is a happy, healthy, breastfed toddler who amazes us every day. I hope for this next child we’ll be able to have an easier pregnancy, delivery and start to life! So far I’ve quit sugar in natural and artifical forms, except for eating whole fresh fruit. I’m really struggling with nausea though so I’m still having some starchy carbs and trying to survive the first trimester. Have ordered your book and am looking forward to learn more.
Well i did the 2 hour gtt… Didnt pass the 2 hour by 1 point. Being that i had GD with my last pregnancy… I didnt bat an eye. But 1 point? Whats your take?
I originally took the 1 hour glucose test on December two weeks ago. They called the next day and said that I had failed. The range at My ob is 60-139. They reported that I was 227. They said as a result of such a high level, I wouldn’t need to even take the 3 hour test as it was definitive that I had gestational diabetes. This did not sit right with me for a few factors based on my lifestyle (more of a paleo/primal diet) and the woman who did my blood draw seemed a little distracted the whole time and even had the needle out of my arm at one point in that blood was pooling on my arm rather than going into the tube. Anyway, I requested the 3 hour test (this past week) since I needed peace of mind. My results were as follows
-Fasting range 60-92. result 102
**I took my blood sugar (with the glucose meter) 1 hour before I left for my test and the fasting number was 88 so the number they reported didn’t make sense to me
-1 hour range 60-179. result 145
-2 hour range 60-153. result 114
-3 hour range 60-139. result 76
I guess my question is, the whole thing doesn’t make sense. What do you make of it? My conclusion was that possibly someone reported the wrong number for my initial 1 hour glucose test and maybe it was supposed to be 127 instead of 227. Wouldn’t my number be much higher on the three hour glucose test at the 1 hour reading since it was 100g of glucose rather than 50g like the 1 hour test and also be higher because glucose levels naturally rise the further on in pregnancy you are? I’ve been frustrated with my OB practice and almost didn’t go back for this second pregnancy and this is just another thing that makes me question my decision to go back this time… if you have the time to give me your thoughts on the situation, I’d appreciate if very much. Thank you!
I’m really not able to give personal medical advice outside of a formal dietitian-client relationship. If you’re interested in understanding your results, what this means for your pregnancy and want my input, go here.
Hi! I eat really well too and lower carbs and very minimal processed foods. My 50g test came back at 144. I didn’t want to do the 100g so I opted for home monitoring so far I have been in the 80s- low 90s (couple
Times with higher carb meals) 2 hours post meals . Fasting between 77-80. I use the relion ultima meter. Do you think this is accurate? Thanks!
Sounds similar to my experience.
I failed the 1hr with a 191 I was sure I would fail the 3hr but I didn’t, I passsed! my fasting was 83, my 1hr was 177, my 2hr was 124, and my 3hr was 115.. can you help me understand how my results were so different from the 1hr
The one hour test is not a fasting test, meaning it can be affected by what you ate prior to your appointment.
Hi Lily,
Thank you again for your continued work! I’m so glad you will be teaching at some midwifery conferences! What are your thoughts on a fasting and 2 hours post prandial option with 75g dose of real food? Also what are your thoughts on the 50g test alternative with jelly beans.
Jen
Good questions, Jen. Fasting blood sugar is definitely helpful to measure, especially given that even very minor elevations in fasting blood sugar are linked to a higher risk of macrosomia and fetal hyperinsulinemia (see the HAPO study). The jelly bean test or 75g carb meal has never been compared to a 75g glucose tolerance test in the research. I’d be more inclined to have a woman monitor her blood sugar for two weeks and include some high-carb meals during that time. That way you get much more information and a woman can see in real time how her blood sugar responds to different meals/meal composition.
Would’ve been interesting to see how you would’ve responded to the 3 hour OGTT. I had almost the same numbers as yours(1 hour, fastings and post pranial), but was labeled GD because I failed the 3 hour too.
Hello Lily,
Is it possible to fail the 50g (not fasting) test but pass the 75g test ( bloods drawn fasting and 1 & 2 hrs after nasty drink)?
This is my second pregnancy. I had gestation diabetes (glucose intolerance controlled with diet alone) during my first pregnancy. This time around in my first trimester I decided to test my sugars 1 hr after a higher carb breakfast and got a 9.9. This prompted me to ask my midwife for early testing. So unfasting I did the 50g nasty sugar drink. Got a 9.something 1 hr later. She sent me for the 75g and I passed. I’m really confused.
No one seems to have enough indepth knowledge to answer my questions. Thanks for any clarification you can give. Genna
Hi Lily,
I was diagnosed with GD 3 years ago during my last pregnancy. I got a 147, and I believe the cutoff was 140. I failed the three hour as well.
My fasting blood sugar was always in the 70s. I rarely exceeded the the maximum of 140 and usually tested in the 120s 1 hour after my meal. I tested for the rest of my pregnancy and controlled my blood sugar on diet alone. Since then I’ve lost weight, about 8 pounds (I wasn’t overweight to begin with) but my current BMI is 19.7. Three years ago my BMI 21.1, when I began my pregnancy.
Anyhow, I felt more confident going into the test this time. I ate almonds and cashews three hours before the test, I was concerned because I was hungry when I drank the drink, but figured it would be fine. Well, according to my glucose monitor I failed spectacularly with around a 250. I haven’t received the official results yet, but I would be floored if they were any different. About an hour and a half later my glucose meter read 175. I went on a walk and when I got back my 2 hour result was 70. Back to fasting.
I’m devastated and so confused. Prior to this test I’ve had my Hemoglobin A1c tested twice. Once last year in April, it was 5.5%. And then again at the end of December, it was 5.2%. I got pregnant 4 months after this test was done, and I continued eating the same way I did in December, which was mainly vegan. I try to adhere to a mostly Vegan diet, but I’m definitely not a vegan. I eat meat maybe once or twice a week and try to keep dairy about the same. During my first pregnancy I was not trying to eat vegan and ate a lot of meat, so protein doesn’t seem to be my issue.
Do you have any advice or ideas about what is going on? My hemoglobin A1c is good, my fasting blood sugar is good, I eat a fairly good diet, and my weight is good. I feel so defeated.
I’d definitely follow up with your doctor and home monitor your blood sugar closely in the meantime. Any reading over 200 can be considered diagnostic of type 2 diabetes (though lab readings with a venous blood sample are necessary vs. a finger stick to make that conclusion). A1c is a not a perfect measure and can be inaccurate for a variety of reasons, like anemia. In short, definitely follow up with your doctor to ascertain what’s going on, but know that it can be managed. Best of luck.
I’m a labor and delivery nurse in a high-risk L&D unit with several years of experience in a multitude of both and high and low-risk, as well as urban and rural settings and am currently in graduate school to attain my MSN degree and license as a Certified Nurse Midwife. I’ve held the position of Childbirth Community Educator. Although health professionals like myself truly strive to help our patients make healthy and educated decisions about their pregnancies, I’ve found that blog posts like these tend to send other pregnant women reeling. You sound like you lead a healthy lifestyle so you’re likely to be low-risk. However when an OB or CNM cares for all types of women, we rely on various screenings and diagnostic testing to ensure that nobody falls into the cracks. It’s been my experience that some women get hung up on their pregnancies and deliveries going a certain way (in part from what they read online) that they force themselves into these cracks and decline treatment for complications that they truly have, but wish they didn’t.
Glucola is nasty-tasting, I feel you. It has things in it, okay. I’ve been researching plain-old Coke (caffeine-free) as an alternative. Not everybody likes coke. The idea is to attain some level of consistency to the test, while working within an office setting where certain amounts of supplies must be ordered within a budget. Is it perfect and ideal for everyone– probably not.
The glucose challenge is the first step in the screening process and that is why practitioners will follow-up with the 2 or 3-hour. There are a number of patients with poor attendance of their prenatal visits that may skip this test due to inconvenience, as well as non-compliant diagnosed gestational diabetics, who do not follow a diet to control their blood sugar, do not test themselves at all, “forget their logbook at home,” and do not take the oral medications or insulin prescribed to them. You can imagine this is frustrating. That said, testing yourself several times a day at home for several weeks in lieu of the 1-hour GTT seems like over-kill.
The biggest problem I have with this post is that you blamed the sugar in your soap for your high results. In the hospital setting we use rubbing alcohol wipes to clean the finger before the test, wipe away the first drop or two or three of blood with gauze, and then apply the strip to the finger. Alcohol is sugar so not doing this will result in a higher number. If you were to do the test accurately with this step, it would reflect a true reading that is not elevated due to the soap.
Yes, if you are health-conscious and avoid sugar then the glucose test itself might affect you differently than a person who follows a different diet than you. It’s important because normal physiologic changes in pregnancy which cause mild fasting hypoglycemia, post-prandial hyperglycemia, and hyperinsulinemia occur to ensure a continuous supply of glucose to the fetus. Insulin is a hormone, and changes in levels of estrogen, progesterone, human placental lactogen hormone, cortisol, and cellular immune inflammatory cytokines through pregnancy affect changes in glucose and insulin production within different trimesters. Whether the woman’s body is not able to accommodate to these normal physiologic changes and results in the pathology of gestational diabetes is random, and does not care what you eat or how much you work out.
Further, the abnormal results of testing, according to the American Diabetes Association and American Pregnancy Association guidelines are as follows:
Fasting: above 95 mg/dL
1 Hour: above 180 mg/dL
2 Hour: above 155 mg/dL
3 Hour: above 140 mg/dL
Random: above 200 mg/dL
I agree with some of what you have said, and I disagree with several points as well. I actively encourage ALL women to get tested for gestational diabetes – that may be via a glucola or it may not be. I encourage you to familiarize yourself with the IADPSG diagnostic criteria, the normal physiology of blood sugar during pregnancy (insulin resistance is a normal phenomenon of pregnancy; hyperglycemia after meals is NOT), and to listen to some of the dozens of interviews I have done on gestational diabetes (or read my book) before jumping to conclusions about what I stand for. This post on gestational diabetes is a must-read, especially for clinicians.
While I understand the limitations serving people with different goals and levels of understanding, many consumers of ob/midwifery care are seeking better understanding of testing and options and are very capable of sifting through information. A one-size-fits-all approach will not work for the new generation of informed consumers who want customized care. We are educated, informed, and proactive about our health. We are seeking providers who treat us with respect and are willing to take the time to inform us and have real discussions that are customized to our specific situations.
Above comment meant as a reply to Jessica’s comment.
I also failed the glycols 1hour screen. My maternal-fetal medicine doc said, “the good news is that you really failed and we won’t have you do the three hour.” I was glad for that because, like you, I do not feel well when I have that much sugar. And fasting would probably be even worse. I was at 201 an hour after chugging the 50g glucola. Prior to this pregnancy I put myself on the paleo diet and stuck to it pretty closely for about 3 months. It was pricey and took a lot of work. I considered sticking to it through pregnancy but when the nausea hit at around 7 weeks, I gave up.
All of my fasting numbers are in the 70s, although I do have one or two in the 80s in the last three weeks. I had one 1-hour post meal reading in the 150s. By 2 hours it seems that I’m always down to the 90s. I’ve had a few in the mid 120s after 1 hour and it’s always when I’m testing out a “treat.”
So I’ve questioned what all this means and been dumbfounded by some of the advice that’s out there about eating more carbs just to be put on insulin. I’m not following paleo now, but because of that, I felt comfortable right away with eating less carbs. And my numbers show that this is working for me.
So, do I really have gd?
I just received my test results yesterday, I failed by 4 points. My score was 134, my doctor doesn’t have her patients do the 3 hour test after failing the one hour one. We just get referred directly to a diabetic doctor. I’m a little frustrated with this because I know many women will fail the first test, and then pass the 3 hour test with flying colors. I guess I just don’t want to have to treat myself like I have diabetes for the next 12 weeks of pregnancy if the first one hour test isn’t enough to actually “diagnose” someone with GD..ya know? I’m very conflicted right now with how I should proceed. Maybe I will just do something like you did with your 2 week experiment and see how I fair with that. On a side note, I really enjoyed reading this blog post! 🙂
It’s not evidence-based practice to diagnose with a 50 gram screening glucola. It doesn’t hurt to check your blood sugar at home (with or without GD), but you may want to seek a second opinion as to whether or not you have gestational diabetes.
Hi Lily, I currently am pregnant with twins and this is my second pregnancy. I passed my 1-hour test with my first pregnancy, never paid attention to my carb intake then and no problem.
I don’t like sweets, rice or bread since childhood. I in general do not eat a lot of carb in my diet, other than fruits (at least 1-2 cups of fruit) and whole grain (about 1/2 cup/meal for lunch and dinner), I sometimes skip breakfast or eat a small snack on the fly for the most part, but I never really counted my carb intake, so I don’t have a good idea how much carb I actually eat whether pregnant or not.
This time around since finding out pregnant with twins, I have been more careful with my carb intake than during my previous singleton pregnancy. And I don’t really crave for carbs just like usual. But to add protein, I have added 1 more serving of fruit, greek yogurt, whole milk, a muffin with pork patty and cheese in the morning, and a protein bar (about the only thing that comes with a substantial amount of processed sugar that I eat), which all contain a good amount of protein needed for twin pregnancy, but also comes with additional carb, which probably pushes my total carb intake to somewhere around 180-200g/day total(?) simply with rough estimation. Even with 200g/day for twin-pregnancy, I feel like I am still somewhat low-carb?
And here I am, failed my 1-hour test of 50g sugar with 164 (threshold 140), and immediately before the test I ate a banana and several large strawberries (ugh); failed my 3-hour test of 100g sugar with 79 at fasting (threshold 95), 196 at 1 hour mark (threshold 190), 201 at 2 hour mark (threshold 165) and 125 at 3 hour mark (threshold 145).
Now I am diagnosed with gestational diabetes but I am so lost. What am I supposed to do with my diet? I already don’t eat much carb to begin with, how am I supposed to cope with that and provide appropriate nutrients to the twins? If you can help shed some light on this, that will be much appreciated!
Very interesting read! I really appreciate all your research-based information and also your story.
I was diagnosed earlier this week at 28 weeks with GD and am still working my way through the panic. I came into this pregnancy with a bit higher BMI than I should’ve, but since the beginning of it I’ve been dairy intolerant, and recently am also unable to tolerate gluten and eggs. I can’t even remember when I had ice cream last (actually, I think it was around week 7. I made a milkshake and got positively sick!!). I’m usually a sweets person but haven’t been able to tolerate most, and we’ve actually started eating Paleo for at least our dinners in the past month.
My GTT 1-hour was 230 🙁 I haven’t seen my specialist yet but I’m curious to know if it’ll be a case of false positive or if I really do have GD since I’ve had so many issues this pregnancy. I’ve only gained 6 pounds so far, which is very unlike my first pregnancy.
I’m actually surprised I didn’t have it (or, that it wasn’t properly diagnosed) in my first. I gained 70 pounds, had an over-9lb baby, she had low blood sugar for days after birth, and I had a very rough postpartum (constantly sick, yeast infections, digestive issues, etc).
It’s all just so strange and hard to wrap my mind around!
Definitely follow up with your provider. I’m unable to give medical advice in this format, but from a general standpoint, any numbers over 200 in pregnancy are worrisome.
I am 9-10 weeks, and after GD in my last pregnancy, I’ve been hoping not to go through that again. Last time around it was always my fasting numbers that were bad (and if I had morning cereal, that never helped).
Well, I just took the 1 hour glucola 2 days ago, and I knew I probably failed because I was wiped out at my 2 year olds bedtime the last 2 nights – like seriously wiped out. I don’t eat sweets in general, and I am pretty good about avoiding processed foods, etc, (but not always about eating noodles). I was even 8lbs less at start of pregnancy over my last go round. (but still very slightly over normal BMI).
However, my genetics are stacked against me. Both my mom and her mom had progressively bigger babies (and likely GD thought they didn’t test for that then), and my grandma had hypoglycemia.
I did fail the 1 hour – with a 173, and they wanted less than 140. I’ve refused the 3 hour, and my type A engineer personality will do a good job at two weeks of data collection. They are asking for fasting numbers and 1 hour after starting each meal. Is there any reason to collect 2 hours after as well? Advice for data collection, reading, etc is appreciated. I’ve really appreciated this blog post, and wish I’d found this site the last time around.
Anything I can bring to my doctors office for consideration is appreciated. I’m in Ann Arbor, MI so they are open to reviewing anything I might bring them.
At my doctor’s office they told me to fast overnight prior to the one hour 50g test. I did and failed (160). I’ve since read that I shouldn’t have been fasting prior to the test. Could that have interfered with the accuracy of the result or could it mean that the test result was actually even more reliable because I hadn’t eaten?
and what was your result after the 3hr test?
Lily, thank you for this post. I am still frustrated (at 29 weeks) that my midwife discredited my request for an A1c panel at my 8 week appointment. I had done some research early on, but in the moment I felt I was “overpowered” in the hospital environment. I wish I was more empowered to stick to my request – but it also scares me how LITTLE healthcare professionals know about nutrition. Someone like me, who did NOT go to medical school has to do research and ultimately curates evidence-based criteria and has to bring this to their attention.
Long story short – this post was very helpful for me to see your experience, as I am also eating a low-carb-high-fat diet, and have been doing so now for 6 years and going. I have been told several myths (from your 9 myths about GD post) about GD and it was as if they just picked it right from your other post.
I opted out of the 1-hr 50g test (with a lot of lecture, appointment with a dietitian) and will be monitoring my blood sugar levels at home just as you did after your 1-hr result.
I have wondered at times too whether my fasting glucose levels are “too low” ! Appreciate the information shared in this post as I can relate, as I eat a LCHF/keto/whatever it is called these days – diet of real, nutrient dense food.
My fasting level was high this morning at 92 and that surprised me – I will check the soap (ha!) 2 hours after breakfast the reading was 87. It was interesting to see you did a little bit of “stress testing” as well with some meals having a higher carb-count. I may do this as well as I am curious, and will do sometimes a 1hr plus a 2hr reading – just for my own knowledge.
Thank you again! I just discovered you via a Diet Doctor post and will be watching your lectures and reading more of your work in the days to come.
Hi Lily,
Thank you so much for the information on the blog! I too just received a false pos on my 1 hr OGTT, with an A1c of 5% and all normal blood sugars (70-80s), both fasting and after meals when checking on a home monitor.
I am seeing my healthcare provider next week to discuss the results. Could you briefly explain why these false positives can occur in healthy women on a lower carb diet during pregnancy? She is not aware of this potential phenomena.
Thank you for your time!
The pancreas adapts insulin production to a person’s habitual diet. It’s been documented since at least the 1960’s in the medical literature that a lower carb diet can lead to inaccurate results on a glucose tolerance test. I delve into this topic in detail in this interview with Robb Wolf.
Hi, I was diagnosed with Gestational Diabetes with my first child, and hypoglycemia with my second. With my second my sugar levels dropped to a 20 at the 3rd hour, my doctor was very surprised I did not end up in the hospital. I ate pretty much as normal with my first after the test and tested my blood sugars after all my meals and they seemed to be normal side note: I probably eat for carbs than I should but I hardly eat sweets. I never tested my sugar levels with my second. My first was 6 lbs 7oz and my second was 7lbs 13oz. I’m now 35 weeks with my 3rd and I’ve been avoiding the glucose test like the plague, I finally did the one hour a few weeks ago and my sugar levels were 180. Now they want me to do the 3 hour but i’m Afraid of actually ending up in the hospital if they do drop really low by the 3rd hour and I get sick every time I even go a few hours without eating and don’t want to do the fasting. Any advice you could give me? Should I just go ahead and do the 3 hour test like tiny doctor wants?
This is a fascinating post, and super helpful. Being 36 years old, I was tested in my 8th week of pregnancy using the 1 hour glucose challenge (non fasting). My # came back at 204 and based on that, I was told I met the criteria for having diabetes PRIOR to pregnancy and was sent to diabetes education and am now monitoring with a glucometer and a “gestational diabetes diet”. I’m showing all very normal numbers except for one fasting of 97 (but I believe I exceeded the 10 hr window). They ran an A1c and it came back normal but they are sticking to the treatment plan until I deliver and numbers show otherwise. The doctor even said, “I don’t think you have diabetes but we need to do what’s best for baby.” Of course, I agree! But as a 112 lb, 5 ft 7 healthy eater (with the occasional splurge) constantly chasing my toddler – I’m a bit baffled at the swift and hard diagnosis of straight up diabetes. The dietary advice isn’t really much different than my every-day diet. I wish they would be more thorough in their investigation. Anyways, all this to say – your post was insightful and useful and makes me wonder what else I should be asking my doctors, or perhaps my GP. Any suggestions?
I am hypoglycemic, and At the time of my first pregnancy, I was eating a nearly diabetic diet since I was caring for my mother who has Type 1. I took the 1 hour glucose test and my results were 160. However, I was not informed not to eat carbs with my breakfast and I had a half piece of white toast. Also, my weight gain was well within normal range and there was little room in my diet at the time to improve so I was skeptical of the results. But I spent a month avoiding any sweets and ate smaller portioning of food. However, I began to get dizzy and felt like my sugar was dropping more often than it should (again, I am hypoglycemic) I began tracking my blood sugar for 3-4 weeks, 3-5 times a day before and after meals. My blood sugar was usually around 70 in the morning before eating and never went above 120 during that month of time. These were my results after spending a month thinking I could have GD because I refused to do the 3 hour test after having a previously awful experience with it. Oh—and my baby began measuring behind my next visit after switching to smaller portionings and less carbs, and I found that I wasn’t eating ENOUGH because I DIDNT have GD. Once I went back to eating my regular portioning and not being so stringent on cravings if they were carbs, baby caught up and I felt much better. And I delivered a very healthy, 6 lb 13 oz baby boy. 🙂
I am still skeptical of the test as I literally just drank it again as I’m expecting my second in 12 weeks, but my diet has not been as good this go round and I’d like to see what my results are when I DONT eat toast with my breakfast right before chugging a gross drink.
I live in Australia and we do the 2 hr 75g glucose test. I had GD in my first pregnancy (failed the 1 and 2 hour levels) but stayed diet controlled.
This pregnancy, I passed the test at 16w then failed it (only the fasting level) at 28w. I also have HG so eating has been a challenge my whole pregnancy. I was so disappointed when I failed the fasting level this time. After I failed I started monitoring my bsl. My after food levels were fine 95% of the time… bread and refined sugar cause issues but I don’t eat them often. To try and control my fasting levels I tried walking at night, tried eating supper, tried not eating supper, tried lower carbs even more during the day and nothing worked. My usual average carb intake per day this pregnancy has been about 100g.
I was eventually put on insulin for fasting and was devastated because it meant I had to change hospitals. I also feel like my body failed me. But I’m now 36w and this journey is almost over.
Thanks for all your blogs and information. I love that you love to research and share what you learn. It has been so helpful for me in understanding what GD is and the things I can do to try and help.
Thank you for sharing your experience. In one office I work in I was out voted and they use the 1 & 3. By the time I see these patients it’s too late overall. I do my best to educate the patient and I’ve given up on the OBs in the office.
At two other clinics webuse the 1 step 2hr. Rarely do I see a false positive but it does happen occasionally. Usually those patients learn about carbohydrate metabolism so it’s not a total waste. In addition, the majority are GDM so it’s worth capturing those patients.
Both offices use a HgbA1c before 14 weeks Gest and I am thankful to have that data.
With all that said, I’ve had a few patients refuse the glucola, as well as, gastric bypass patients that cannot take it so home SMBG is the best next option. Again, I see it as an opportunity to teach the patient (& OB).
I LOVE THE SCIENCE BASED INFORMATION YOU SHARE ON SOCIAL MEDIA!
Sounds like those other offices are using the Sweet Success guidelines, a program I used to work for. Bravo!
Yes, bariatric surgery patients can’t do a GTT/glucola, so home blood sugar monitoring (or some new research exploring the use of CGM) is an appropriate alternative.
Had both the 1-hour and 3-hour glucose screening tests done. Needless to say, my body did not react well to either the 50g or 100g glucola drinks, especially the 3-hour which was done on an empty stomach. Good news is even though I failed the 1-hour test (137, which was 3 points high for my OBGYN), I passed the 3-hour test. Did notice my blood glucose levels were slightly elevated and outside the normal ranges mentioned in the article. I do have PCOS which has been shown to cause insulin resistance in women. Not sure if this is what the test is showing. Would appreciate any of your comments/advice on best ways to manage insulin resistance while pregnant.
I had a 2 hour GTT done at 28 weeks pregnant in Australia. They recently lowered the cut offs for diagnosis. My results were:
Fasting: 5.1 mmol (They want less than 5.1 mmol / 90mg/dl or less)
1 hour: 9.7 (They want less than 10.0 mmol / less than 180mg/dl)
2 hour: 7.4 (They want less than 8.5 mmol / less than 174mg/dl)
I was diagnosed with Gestational Diabetes based on my Fasting being 0.1 mmol above the cut off.
Then the targets given to pregnant women in Australia who are home monitoring their blood glucose levels is to keep fasting below 5.1 mmol / 90 mg/dl or less, and then 2 hours post meal 6.7 mmol / 140 mg/dl or less.
Well, at first I thought, gee, I only just scraped in with this diagnosis. How seriously do I take it? But then I just felt thankful to have been given a warning that I obviously have a level of insulin resistance worth paying attention to considering insulin resistance seems to be the root of most of our chronic diseases. So having this chance now to change my diet might save me from future health problems that would have hit me sooner and potentially with no warning.
So I started eating much lower carb. Struggled a bit when testing for ketones during the pregnancy when I would get over 4.0mmol sometimes. Not sure what I was supposed to make of that, but my OB told me I could ignore that, so I did.
As the pregnancy went on (I’m 37 weeks now and scheduled for a C-section in 4 days time!), I noticed my morning fasting level was going up slowly no matter what I did diet-wise. It got to 5.6 mmol / 120 mg/dl a few times when I was finally put on nightly insulin and it still took a couple of weeks to bring it down, but even with the 22 units of insulin I am currently on, I still wake up regularly with it just over 5.1 mmol. And my post meal readings, well, to me, when I ate 4 VitaBrits with a bit of honey (breakfast cereal) and my blood glucose spiked to 9 or 10 (180 – 200mg/dl) and was still over 8 mmol / 144mg/dl at the 2 hour mark, I appreciated just how sensitive I was becoming to carbs in this pregnancy. By 33 weeks, baby was measuring 2 weeks ahead. Not sure if he has continued growing at that rate. Will find out in a few days I guess!
Anyway, I’m supposed to have another GTT at 6 weeks postpartum and I am balking at the idea because I am now eating low carb and don’t want to start all over again with sweet things. I am assuming I have a level of insulin resistance that could be prediabetes already, or maybe not, but I’m going to tell myself that I had better not be complacent and just go back to eating how I was before. Whether or not I need the GTT to scare me in the right direction, or whether I just take things more seriously and just start looking after myself by eating low carb from now on, to me it makes sense to use the diagnosis of Gestational Diabetes as motivation to change for good. I may find I even pass a GTT once the pregnancy is over. But I’d rather not let that make me think it’s okay to just go back to all the carbs and sweets I was eating. I feel I need to take it seriously. I am 44 years old now and they say 50% – 70% of women with Gestational Diabetes go on to develop Type 2 diabetes within 15 years or so, but since I’m not in my 20s, that could be just around the corner for me, so it’s not worth the risk of returning to my old ways of eating. I think most of us know when we are eating food that is not good for us but it’s easy to keep our heads in the sand until we get a disease. Why wait for a disease to catch you if you can do something about it now?
By the way, I feel that many pregnant women who are not overweight and eat healthily but who still fail the GTT and find they have slightly elevated fasting levels may not be seeing the bigger picture if they are just sceptical about their diagnoses.
We assume that eating “healthily” means following the food pyramid suggested by the government with “healthy carbohydrates”, whole grains etc. at the bottom of the pyramid – meaning eat those things mostly, but I think that is being disproven again and again and really, the amount of carbohydrates that we are encouraged to consume, whether they feel healthy to you or not, is excessive, so many of us are ending up insulin resistant. And insulin resistance seems to be the precursor for most of our chronic diseases. So rather than questioning the GTT results, just reconsider the amount of carbs in your diet and try to lower it by increasing a combination of healthy fats (from animal sources and not seeds), proteins and non-starchy vegetables, and you’ll probably be doing yourself a favour.
Hi
I “failed” the 2hr test my last reading was 8.1 cut off is 8.0!(Australia) I was so angry at myself..I tested my BGL 4 times a day (and more because I became obsessed) and never had a high reading. My readings were 3.9-4.1 fasting and 4.5-6.4 after meals at 1 & 2 hrs post respectively. It actually ruined pregnancy for me because I was clock watching and over testing trying to “catch out” my alleged insulin resistance! The diabetes educator said there was no point seeing me because everything was normal. The obgyn didn’t review my at home results (I had to remind them) because they were normal. If Iam going todo all this testing they may as well humour me and have a look at my results!!
I was induced for fear my placenta wouldn’t last the trip and my baby was a very normal weight 7lbs 3oz.
Tested until I ran out of test strips post partum..still normal. Too anxious to have my post partum glucose test..I’ll do it soon I guess
Bit of over medicalised treatment which ended up causing me a great deal of anxiety and stress
My doctor had me take the 3 hour test at 10 weeks after being 2 points high on the 1 hour test. My fasting was at 99 but I tolerated the glucose and was within the normal range. I have been testing my blood sugar regularly since then and have had fasting blood sugar mostly in the 80s (never above their threshold of 94) and under 120 one hour post meals (usually between 85-110). So, my doctor and I decided I should take the 3 hour test again so that I wasn’t categorized in their system as having GD (I’m now 28 weeks). Well, that plan backfired. My fasting was 79, but the one- and two-hour post glucose values were high. By 3 hours, I was in the normal range. I eat a low-carb, high protein, high nutritional content diet, but now I’m frustrated. I have expressed to the health care providers that what matters is my regular, daily levels of blood sugar, not the results of a test that is not ecologically relevant and has little external validity.
I know I’m in charge of my pregnancy and health care decisions, but how do you suggest I proceed if they begin to threaten me with fears of a “big baby” and push for induction?
Hi Lilly,
This GD thing has had me all over the google place lol. 3 years ago I was pregnant with baby nr 3. After a 10 year hiatus of nr 2. I have been gluten intolerant for over 20 years and ate very few grains or even potato at that point pre pregnancy since it juat makes me feel like yuck. So when pregnant with nr 3 they did a ton of bloodwork throughout. Fasting was always in the 70s or 80s and A1c at 9 weeks was 5.2. Fast forward to the 1 hr glucola. At this point I have stopped eating all grains, table sugar and starchy carbs to negate severe nausea and stomach issues. Diet consists out of fruit, veg, nuts and seeds, meat and eggs. Only honey and Maple syrup for sporadic sugar flavoring. I do suffer from low blood pressure (always have) so I actually do add pink salt to my water (only thing I drink). I fail the 1hr with an 180 some rating. Never happened before but ok. Week later go for the 3hr 100mg test. Take the blood, drink the drink. 45 min baby goes nuts and then completely quiet. He stopped moving completely. Take the other blood intervals and feel like crap. On the way home I shove my high protein snack in me as I start shaking and freaking out. Baby is still not moving normal, feels like a slow motion movement when he does move and he’s normally a karate ninja. Office says its fine he acts that way. Come home and have a total sugar crash. After eating my nor al whole foods and feeling back to normal the day passing by agonizing slow since the peanut had stopped all movements on the ride home. 12 hrs after swallowing the first sip he finally starts stirring in slow motion amd is back to normal bu the next morning. I however am not. I have several sizeable patches of a breakout. Back of the knees, ankles, chest, around my.face. They are thick, hot and remind me of a systemic poison ivy attack (I’m highly allergic to it) within days there isn’t a spot on my body not showing a thick raised cluster hive or individual bumps. The itching is excruciating. Nothing helps. I get the call I have GD. Something doesnt sit right. I’m having a full blown allergic/histamine attack here. Dr. Google comes in and I get a meter and start testing. On my daily diet, nothing notable like your experience. When I eat a half a cup of plain white rice (as a way of testing carb sensitivity and only did that 1x), full blown diabetic readings. over 200 1hr post meal. Normal after 2hrs. Fruits are fine, apples dipped in honey are fine. But starchy carbs, chocolate, and peanuts spiked. They were very specific food groups. After 5 weeks of absolute hell, for it didnt get much better and I would wake up at 3am daily for a 2 hr scratching session and in tears. Someone finally at the doctors office regocnized it and said i was allergic and stopped pushing for me to go and eat the diabetic diet since I felt it would kill me. Referred to an endocrinologist. Ran more blood A1c of 5.4. Explained what had happened. Had a 2 fastings off 100 and 105 in 2 weeks amd she said to go get insulin! I was appalled. I asked if we couldn’t addres this whole body systemic histamine freakout first for I was desperate for relief. She agreed finally and gave me from that Thursday until Tuesday to report at the clinic. I asked for an antihistamine and she prescibed 2. Both which contained corn something I wasn’t about to take again and had consulted her about all the while she claimed that they were corn free. Not according to the listed incredients. Dr. Google to the rescue again. Plain clear Benedryl in capsules without any.food coloring etc was deemed safe. After asking both offices (obgyn and endocrinologist) was given the clear that it wouldn’t harm the baby and wouldn’t affect my sugars.
I have NEVER felt such a relief until 20 min after taking the 1st dose with some food. The baby agreed. For he became crazy active. 2 hrs later sugars were back in the 80’s. An average 20 point drop 2hr post. I kept taking the benadryl until Sunday night and was completely healed up (except for some scabbing) no more hive plaques by monday morning. All the readings in general had come down. Not that they were high to start with except fasting towards the end before starting Benadryl. Called the endo and she said not to come back. I kept an extremely vigilant eye on what I ate. Talked to the office and they felt it wasn’t GD but a major allergic reaction. Had a healthy 8lb9oz baby boy just shy of 40 weeks vaginally. Never gained excessive weight. Did fingersticks as soon as he was out on him and me and we were both fine.
I thought the whole ordeal was over. Our son however turned into a colicky mess about a week after birth. I had resumed eating pre pregnancy and wasn’t sticking to the grain free, peanut free, table sugar free, starchy carb free. He was breastfed but super gassy. Gained well but at 6mo ths could only tolerate mangoes. Everything else , fruits, grains/starch, white meats produced cramping, bloating, diarrhoea, a facial rash and bleeding bum. We were a our wits end. We finally figured out he could eat duck egg yolk, oils like butter, fermented dairy and red meat. I finally weaned him at 20 months. He was able to eat everything after 1 month post weaning. I on the other hand had gained all the pregnancy weight (30lbs) back, was hurting physically and just exhausted. After weaning I didn’t lose the weight quite yet but realized I needed to cut my diet back down again. Now preggo with nr 4. The blood sugar meter didn’t show it between the pregnancies (the scale and how I felt did, something that didn’t happen with nr 1 and 2) but its showing it again this time. I feel I have now narrowed it down to sucrose intolerance/histamine intolerance but am unwilling to eat the offending foods for sake of testing since eating them could have auch a potential allergic reaction that I don’t want to relive. Our son was textbook for congenital sucrose intolerance although it stopped after breastfeeding. So that makes me the culprit.
Have you ever had clients where food was so extremely reactive? And do you have any food guidance for the Dawn syndrome for someone like myself? If so I’d love to take your course but am hesitant since Iam so far outside the norm. And this time I know better and finally feel at ease. A very clean diet, don’t want to call it strict. Only meats (whole ones without solutions injected, marinates etc), veggies, fruits, whole nuts (almost all butters etc have sugar etc) dried fruit. I haven’t gained any weight (down 4 lbs and 25 weeks along) which was concerning at first but knowing I’m starting at the weight I usually end at not a bad thing either. Baby is growing great and another kung fu master. I check my sugars every morning and during the day if its a “new” food. They are always in range thankfully. Not doing a glucola challenge this time OR EVER again. The midwife has agreed to let me eat my foods. Even subbing the potato or bread for a banana (since I don’t eat the potato or bread anyway).
Hi, I came upon this because I feel like I am being wrongly “labeled” GD.
I questioned it because my fasting was normal (80), my 1 hour was normal then all the sudden the 2 hour spiked over “normal” and the 3 hour was borderline at exactly 140. why I questioned it was because the 1 hour was taken precisely at 1 hour, the 2 and 3 hour ones were drawn at min 45-48. the nurse in the office said that they call you that early but by the time its drawn its an hour. Not so. it takes literally a max of 5 min to do this from waiting room to lab draw I timed it and I am also a nurse and know it doesn’t take me 15 minutes to ‘set up’ or draw one single lab.
so now I have to see an endocrine person and I am not really happy about this. would you suggest I do home screening to bring in some numbers?
Thank-you so much for this article. I failed both the 1 hour and 3 hour with this baby, but I knew I was eating healthy so I was surprised. I’ve been taking my blood sugar numbers now for two weeks and all are perfectly normal. Fasting is always in the 70s. When the dietician met with me, she told me I needed to eat more carbs – a lot of the carbs on her list were simple, refined ones. And that most meals should have a balanced amount – around 45g. I do eat carbs – whole grain sourdough bread, beans, etc. but not nearly the amount recommended, so I’m so glad to hear what I’m doing is fine.
I’m in the same position as you were. Failed my 1 hour with a value of 139–my doctors office considers >134 abnormal. I am a nurse and bought a glucometer and have been checking my 2 hour posts and fasting blood sugars. All have been within normal limits. I too come from a background of low carb / lower car diet. I’d rather monitor myself at home and nourish my body with healthy low glycemic carbs then worry about actually having GD. Thanks for posting this article! It makes me feel far less crazy about doing it my way.
Thank you so much for this article. I’ve always tried to eat a healthy diet (basically low carb without realizing it). Well with my 2nd pregnancy I again ate my normal diet and with chasing around a 2 yr old I found myself skipping breakfast and not snacking throughout the day; only eating my regular meals. Well needless to say I failed the 1 hr glucose test with a 162. My dr. didn’t really seem concerned because I was not high risk. So I went ahead and scheduled the 3 hr glucose test and still followed my normal low carb diet (with the occasional dessert and fast food outing 🙂 but overall I try to eat healthy especially since this is my 2nd baby.
I went for the 3 hr test and drank the 100g glucose drink and immediately realized this isn’t working well with my body. By the 2nd blood draw I almost passed out and knew I was not gonna get good results. Low and behold I got my results and the fasting was 69, and all the blood draws afterwards were in the 200s! Therefore I got the diagnosis of GD. But I couldn’t shake the feeling that this may have been a misdiagnosis based on my low carb low sugar lifestyle. I’ve been monitoring my glucose levels at home and all my fasting #s have been in the 80s and that’s after 10-15hr between dinner and waking up. All of my other readings have been below 120 after 2 hrs post food. My dr has never expressed any concern with the high #s from the glucose test and as such I’ve emphasized that I believe I was misdiagnosed especially knowing my fasting at the 3 hr test was only 69.
What are your thoughts on this diagnosis? I hate having this label put on me especially after tracking my own diet and getting no where near 200 blood sugar levels 🙁
Thank you so much for sharing! I failed mine barely with a 143 on a low carb diet. I was so frustrated because I try very hard to eat reasonably well and exercise. From what I can see I have no risk factors for GD. I also failed the one hour with my first pregnancy and passed the 3 hour no problem. I’m hoping that I pass the 3 hour again. I’ve got a new OB this time around and feel like she is going to think I’m not taking care of myself or my baby.
Hello Ms. Lily Nichols,
Thank you so much for this post. It might be really old (I didn’t see a date). It is nevertheless extremely helpful. I have to take the glucose test soon and I was looking for a “polymer glucose solution” what they give most women is a “monomer glucose solution” which has more side effects (Evidencebasedbirth.com). Juice is a polymer glucose solution, but the sensitivity is not as high. I would opt for organic jelly beans if possible, but that is not an option at my practice. I’m so glad that you pointed out how this test is not very effective, but it’s all we have. There needs to be a better way. Chugging down 50g of sugar in 5 minutes (no one does) with so many variables shows how this 1976 test needs updating. Thank you again for posting your experience!
I think the tests for GD are complete garbage. There is absolutely no medical judgement used by doctors. Seriously, I pay for their expertise, but if all they do is read results to me, what am I paying them for? I’m s relatively intelligent person…I read and understand test results by myself.
I eat a whole food, plant based diet, so tons of dark leafy greens, whole grains, legumes, vegetables, and yes, fruit. This is pretty much the diabetes-proof diet. I basically eat no refined or added sugars (by any name). So yeah, when I’m pumped full of 100g of refined sugar in less than 5 minutes, it’s not a surprise I didn’t pass this ridiculous test. My fasting number was 70, well below the passing number of 94, at one hour I had a 180 where passing is 179, two hours I was under the 154 passing number with 148, and at three hours I had a 140, compared to the 139 passing number.
When someone whose diet is so well balanced that as a vegan, no iron supplement was needed, and has been told to gain more weight throughout their entire pregnancy misses the mark on the three hour test by literally one point, some amount of judgement needs to be exercised by the doctor. IMO, it is inexcusable to diagnose a woman with GD, and then also have to send her to the perinatologist to check for IUGR, without ever having been on insulin or any other medication.
Women who carry twins (or more) are more likely to be diagnosed with GD, even if they are of normal weight and healthy before pregnancy. Twins+ are usually born early and small. Has anyone considered studying whether a GD diagnosis for women carrying multiples is possibly linked to that? Maybe their bodies, and nature, are smarter than doctors, and they need more sugar in their blood to allow the babies to grow to a normal size. Maybe we should test to “normal” glucose levels, not “pregnancy” glucose levels. How many otherwise healthy women who were diagnosed with GD who birth very small babies would have passed such a test? Would their babies have been closer to average size?
Anyway, I could go on and on about how ridiculous this diagnosis is for some people, but it would become a novel. We need to do better. We are failing women and their unborn babies.
I totally agree with you! I was just diagnosed with GD and I never eat refined sugar and have a very good diet (limit carbs, eat fresh fruit and veggies, practically no sweets) and I am below my BMI. Of course my body is going to freak out when I am forced to drink that glucola drink. Now I am taking my readings at home and my readings are all below the normal range. I think there is conspiracy to get people to pay for more medical supplies for others to line their pockets. It has made me super emotional and worried and I feel like for no reason (7 months pregnant).
What soap do you recomend? I just saw mine has the sugar derived ingredients you listed.
Thank you so much for this post! Very reassuring as I also have 0 risk factors (aside from pregnancy). I Exercise 5x/week, I’m a fellow low carb, low GL RD, Pre pregnancy BMI 21, and appropriate weight gain during pregnancy. I have read pieces of your book real food in pregnancy and recommend it to everyone. I really wish I had read it before my 50-g GTT (“Failed” with 139) and 100-g OGTT (“Failed” with 65, 184, 153, 65). After the first fail I started testing my fasting BG was from 75-85 every morning, post-prandial within range as well. My doctor was not understanding or flexible with alternative testing methods, or possibly false diagnosis. How can we spread the word? This process is so stressful for a first time pregnant mom, and It’s a shame that the test is so antequated and Arguably not appropriate for patients who are so diligent about their nutrition. Thank you for sharing this, such a helpful post!
Can I ask why the ranges for normal are lower compared to someone who is not pregnant testing for diabetes?
Thank you for writing this article. I am in my second pregnancy and have been following a relatively low carb diet. In my first pregnancy I ate plenty of carbs and sugar and passed the 1-hour easily. When I took the 1-hour glucola this time I failed miserably- 171!
I read your article and others about the effect of eating a low carb diet on the glucola results. I ate a minimum of 200g of carbs per day for 7 days before the 3-hour test. I passed on all 4 values!
I’m so relieved and thankful to you for providing this helpful information which helped me understand why I didn’t pass the first time– not because I have gestational diabetes but because I eat a low carb diet. Thank you thank you!!
So glad it was helpful to you!
How would you talk to your doctor if you believe you were misdiagnosed with Gestational diabetes? I like you normally eat well and have a low carb diet. They have had me checking blood sugar levels at home and so far all my fasting levels are between 70-84. Eating my normal my numbers are always well in normal range. I’ve even tried a few really high carb meals, and my numbers come back below 115. I feel like I’ve been misdiagnosed, but I also don’t know how to talk to my doctors about this in a way that I’ll be taken seriously.
So I’m also a registered Dietitian! This is my third pregnancy and I drank the glucola drink last week at 30 weeks and I failed for the first time with a 147. I clearly was shocked and couldn’t believe it. I’ve been running 3-4 miles every day, and I eat whole grains, legumes, vegetables, fruits, and cook at home. We eat chicken and fish sparingly. No processed foods. Since the whole covid thing, they are not doing the 3 hour test so my doctor referred me to the diabetes center. I’ve been so shocked by the whole thing, I don’t even know what to think!
Hi!
What about post pregnancy glucose levels?
When pregnant I ‘failed’ OGTT but was able to keep my sugar levels low via low carb diet, however now, in pp period I get high sugar levels after eating carbs (for example 11 one hour after eating gnocchi).
I did not do OGTT PP and not ready to see the doctor.
Thank you
Hi!
I have been eating a ketogenic diet for over 3 years. Since finding out I was pregnant in February 2020, I have just done more of a modified keto genic diet where I eat lower carb during the week with some carbohydrates such as potatoes along with meals. I was very anxious that due to my low carb diet I will get a false positive on my glucola testing. I just got the dreaded phone call today that I failed my GD test.
I had a feeling I would based on the fact of how my body would react to a syrupy sugary substance that I wasn’t used to after so many years.I had attempted voicing his concerns several times to my OB and was met with absolute resistance saying that the research I have done was not accurate.I’m going to be opting to test my blood sugar at home instead of undergoing the three hour test. I just wanted to reach out to you for any support and advice as I am incredibly frustrated that my voice wasn’t heard prior to being tested with the glucola substance.
Thank you!!!
This has definitely helped make sense of the test for me. I failed both tests but I’m very petite and eat low carb high protein fresh diet. My fasting blood sugar before the test was 75. And then they shocked my system with the drink and I felt awful. I never eat sugar like that and again I’m very small. 5ft 1 inch 100 pounds pre preg and now 108 starting my 3rd trimester. I feel the test was wrong and telling someone who is small like me to cut out carbs is silly as I am trying to gain weight for baby. When I do eat sweets I savor them slowly over a long period of time. The glucola drink is so unnatural and now I’m over analyzing what I’m eating when I should just be eating for baby to grow.
Lily,
I am SO happy my doula pointed me in your direction. I failed my 1 hr screening “so bad (according to the nurse)” that I don’t get the option of a 3 hr test. I am being diagnosed by that one test, starting 4 x daily glucose testing, and meeting with a diabetic educator.
I was FLOORED when they called me. Beside myself. I am a very physically active person and eat a very low carb diet. I was so so upset. I initially was very angry I was not offered a 3 hr test. After reading this and a couple days of self-reflection, I realized, what’s the worst that can happen? I’m sure I have room to improve my diet, keep my baby healthy, and improve my eating habits. And if I keep my blood sugar logs and find that it’s all coming back normal.. then good! At least I know I’m doing the best thing for me and baby.
My doula got me your book and I’m so excited to start!! Thank you for what you do!
I was diagnosed with gestational diabetes after I failed both the 1 hour and 3 hour test. I was devastated and truly felt like a failure. I’ve always practiced good healthy habits – pretty good diet, regular exercise, healthy weight, normal weight gain through pregnancy. I was able to manage my GD through diet and monitoring blood sugars. My fasting blood sugars were almost always below 80 and 2 hours after meals rarely ever exceeded 100. My daughter was a health 6lbs 13 oz baby. I’m a huge believer in diet for management and hate how people scare you into thinking you’re automatically going to have complications or assume you’re unhealthy. I sometimes wonder if I was misdiagnosed. Curious to see what will happen with my next baby. Considering just monitoring my blood sugars from the get go to avoid the stress of the testing and the “failed” terminology. I do feel like in the end I ate healthier than I maybe would have without the diagnosis, learned a lot about my diet and body, and didn’t gain much weight so I suppose there was positives from the experience. Thanks for all your information!!
Hi Lily! I have your incredible book Real Food for Pregnancy and I reference it ALL the time. I also follow you closely on Instagram… I thought I remember you saying you used a CGM during one pregnancy? Did I misremember that? Either way, have you come across any research on pregnant women with low glucose readings especially overnight? The only thing I can find is that if it’s really low (below 40) you might be laying on it and that it’s common for no pregnant active people to be low at night. I’m 19 weeks and wondering if I need to worry about this. I will also raise with my doctor, but I’m guessing they won’t know any research to base their answer on. Thank you so much for all you do!!! I love supporting your work!
Hi, I just bought your cookbook on GD diabetes today and it cleared up a lot for me regarding outdated advice I was given, and I also enjoyed reading this post. I still have a question/confusion around being diagnosed on Christmas Eve after failing the three hour. I eat gluten free, organic, minimal sugar and so my appointment with the dietician was super confusing because she told me to eat 200 carbs a day….after I showed her I’d tracked an average of 90 carbs a day the three days prior to my appointment. Luckily I didn’t follow this advice and have now completely cut out sugar but have made minimal changes and increased activity. My blood sugars have all been fine the past week and a half…any chance you can give me your thoughts on this as I remain confused about pretty much the whole thing! If I haven’t changed much and my sugars are fine is there such a thing as a false diagnosis? I’ll continue checking but would love any input.
This is an older post but I wanted to thank you for putting it up and being so thorough about your experiences! I am an RN in Oklahoma and began immediately questioning why we don’t do an initial screen for GD in the 1st trimester with an A1c when I was first learning about it in nursing school. My own A1c this pregnancy was 5.0 at about 12 weeks and I am currently in the process of doing q4 home blood sugar checks voluntarily at 24 weeks. It is so valuable and fascinating to have the actual numbers in front of me, to have some reference ranges, and to be able to see exactly what foods and circumstances my body reacts to. I was was motivated to take that action due to having had a macrosomic baby my 1st pregnancy despite measuring “normally” by fundal height and having passed my glucola with flying colors. I gained about 40-45 lbs that pregnancy which I think definitely contributed. This pregnancy, I have kept a tighter watch on my weight, my diet, my stress levels as possible (I am a huge emotional eater), and I have had great results. Thanks again for the great info! It’s very motivating to learn about optimal health and wellness when we are in a position to take action.
Hello Lily!! I love your work and wish I had discovered it before December 2020, at 21 weeks pregnant. During that December appointment I was told not to eat refined and starchy carbs – sugar, flour, rice, potatoes, etc. – as I had already gained 22 pounds and was at risk for GD. I got a copy of your book, Real Food For Pregnancy and immediately started journaling my food and keeping track of my carb intake (trying to keep it below 75g and always below 120g per day.) My weight went down about 6 pounds pretty quickly, and I’ve been fluctuating about 5 pounds and maintaining my weight altogether. Yesterday I had my glucose test and failed massively with a score of 151. Speaking with the lab technician gave me some cause for concern, and I was afraid I would fail the test. #1. I did not fast at all prior to the test, and in fact was told by a woman at the front desk of my OB office that I didn’t need to worry about that… but I literally ate breakfast 45 mins before drinking the glucola (your crustless quiche recipe, sausage, 1/2 cup Greek yogurt with some raspberries and blackberries in the yogurt). #2. I drank a cup of coffee in the morning. The lab technician told me she would personally reschedule and come back fasting later. Getting my results this morning have been pretty upsetting. I don’t want to face health problems, but more importantly I don’t want my little girl to suffer any consequences. Trying to maintain some calm before I can speak with my doc. Feeling a bit better hearing your story!! Thanks so much!!
I would love to hear more about blood sugar in the context of reactive hypoglycemia as well. When diagnosed with PCOS my care provider ran a 75g 2-hour glucose test and my fasting was 91 (which felt high to me honestly) and then my 2 hour level was 73 which they marked as a “low value” but later told me was great because my insulin must be “great”. There is very little info I can find on the topic because high postprandial levels are much more common! I have always been someone who has to eat small amounts every 2-3 hours so this is likely part of this. Would love to find some research on this…
Hi Lily,
I’m in the UK 12 weeks in to my second pregnancy. I was diagnosed at 31 weeks with my first but fully diet controlled thanks to your book. My reading were so good that the doctor didn’t believe them.
I wanted you advice on safe blood sugars I’ve been targeted under 5.5 for fasting ( I have a wakeful toddler and I’m really struggling with sleep and sickness so my fasting level are all over the place from 4–5.7)
Post meals are under 7 are these figures at lots lower than US?
Have a GGT next week and feeling exceptionally worried about it.
I just finished reading your book and learned so much! I am pregnant with my fourth and have always passed the one hour test in the past while being on a carb-filled junky diet. After having slightly elevated numbers in the last two weeks with my third baby, I researched A LOT and switched to a strict keto diet a couple months after the birth. I have not cheated for over a year and have stuck in the 20-30g of carbs for most of that time. I make everything from scratch, grass fed pasture raised etc. I have been producing ketones the whole time and had several insulin resistance symptoms improve. Now, pregnant again, I asked to monitor my blood sugar instead of doing the glucose test. But my fasting numbers are usually 105ish! It is my highest number of the day, I take it 30min/1hr/2hr after eating and they are always lower than my fasting number. But because of my fasting number my doctor wanted to go ahead and do the glucose test…I got 170!! They are now wanting to do the three hour and because of my fasting number I don’t have another option that I can think of. I am carb loading but I wondered if you had any other suggestions? It is possible I developed diabetes while on the keto diet since having my last baby?? Thank you!
This was an interesting read. I am in Canada and did a 2 hour glucose tolerance test (which I allegedly failed ie. the ‘normal range’ is 3-5, and I scored 5.3), which I was surprised by, followed by a lecture about diet and exercise from my midwife (insert eye roll). I also eat an organic, low-carb diet (and have before pregnancy), as well as live an active lifestyle. I was wondering how much of a self-fulfilling prophecy that this might be, given that the amount of sugar I was given (75 grams: after 13+ hours without food) is so far beyond what I would consume in 24-48 hours (and yes, carbs are generally a relevant factor). I also question the measure of weight and BMI as benchmarks of determining a healthy pregnancy (or health) and growth of the baby, as there is little differentiation between types of tissue/bone density. It is worth mentioning that I was considered to be slightly toward the higher end of ‘normal’ BMI, but yet again, have always been active, muscular and solid. Furthermore, I find the whole screening parameters, ie. ‘non-white’ ethnicities being more prone to GD extremely off-putting and homogenizing (not to mention the lack of culturally appropriate/relevant dietary guidelines). It’s hard not to feel offended by all this, even if it is well intentioned. But I think you brought up a few great points on the lack of finely-tuned and succinct screening methods (not to mention paranoia-mongers within the medical care profession), and I think one of the best methods we have as pregnant women, is to pay attention to, and tune into our bodies – it’s just too bad that there’s often no real way to quantify our intuition with medical professionals.
Appreciate your evidence-based approach and have been enjoying learning from you via IG and your blog posts. I just returned from the 2-hr test my OB utilizes, having failed the 1hr at 193 but ended up with an 88 at the 2hr mark. Is there any data to suggest those who fail the 1hr. are at risk of a pre-diabetic state? Is there anything those of us who fail at relatively high numbers but go on to ultimately pass the diagnostic portion should be aware of or modify. I strive for a general 80/20 balance, with a focus on whole foods, frequent exercise, with no obvious risk factors but am now left wondering if there is anything I should take action on.
I am a Gastric Bypass patient. It is extremely saddening that most doctors do not consider the glucola test as ineffective in cases like mine. My body no longer processes sugar in the same way. I am very blessed to have a doctor that researched in to the best care for me, but hearing so many bariatric surgery patients get violently ill from the tests, or feel ok during the test and go undiagnosed to have complications later. As post bariatric surgery pregnancies are on the rise, I would love for more information to be available to reduce the risk of misdiagnosis. Is this something you have studied at all?
Hi Lily,
Really enjoyed your posts about the tests. I’m in Canada and I was high risk with twins last time. I passed the two-hour test but not without enormous physical difficulties. All I can remember is sweating and shaking and trying not to throw up for hours, and then feeling like I’d been hit by a car for the next 24 hours. I failed my 1 hour test with this subsequent pregnancy, and I’ve been told to do the 75g two-hour challenge. I’m not allowed to lay down at the clinic for hours because of COVID. The thought of having to repeat the two hour test is giving me so much anxiety because of my experiences from my last pregnancy. I don’t know how I would be able to walk around and go back and forth for this test. Your posts encourage me to speak to my midwife about alternatives like monitoring.
Hi there!
Can you please help me understand how carb-loading the week before would help your blood sugar decrease when doing the 1-hr OGTT? I am just curious. I generally do not eat a lot of carbs, but since being pregnant, I have increased my intake a little bit. I generally stick to fruits and vegetables w/ rice or potato 1-2x per week (as in, 1-2 meals, not 1-2 days, multiple times throughout the day). I’m wondering if this in some way has caused my pancreas to under-react when exposed to 50g of straight sugar (which I would otherwise never consume).
The pancreas becomes adapted to secreting only the amount of insulin needed to cover a person’s typical diet. If one is low carb for a long time, the pancreas is not adapted to produce large boluses of insulin. Eating higher carb leading up to the test allows time for the pancreas to become accustomed to producing large boluses of insulin and can therefore reduce the risk of a false positive. This is explained in greater detail in Ch 9 of Real Food for Pregnancy in the section on gestational diabetes screening.
Hi Lily! Man oh man…I really wish I found your article BEFORE going through with my 3-hour toxic glucose test!! I, like you, barely failed my 1-hour screen (142). This was an absolute shock to me because I’m a former professional ballerina with an impeccable diet (organic whole foods diet rich in vegetables, fruits, nuts, legumes, seeds, fish, high quality lean meats, cottage cheese, yogurt, sprouted whole grains, etc.) that happens to be low glycemic, highly varied, nutritious and unprocessed. I’ve eaten this way for most of my life and will occasionally splurge on sweets, but am extremely conscientious.
I (regrettably) ended up going through with the 3-hour test and ended failing this as well! Truly unbelievable (or perhaps super believable, given my diet and likely intolerance for large quantities of sugar, preservatives and dyes). I’ve now been tracking my blood sugar levels 4 times a day for over a week, having not altered my diet in any way (I eat tons of bananas, honey, dried fruit and other high sugar items) and my levels are all super low consistently!! Fasting is 70, post meals at 2 hours are 70s and 80s, low 90s at the highest. In addition, my first trimester A1c was 5 and I have zero other indicators of GD (minimal weight gain, amazing energy, etc.)!! How do you suggest I present this information to my doctor? I’m afraid I’ll just be seen as another number, but I truly do not think I have GD and I don’t want a misdiagnosis to change the course of my pregnancy with the extreme stress and anxiety it’s giving me. Any input or perspective you can offer would be very much appreciated!
This post was extremely reassuring. I “failed” both the 1 hour and 3 hour test (by like 1 or 2 points) and was put on Sweet Success Program in CA, with home monitoring. I’m only 3 days in to my monitoring, but so far all readings have been well within the normal range and the Sweet Success diet plan doesn’t feel like too far a departure from how I was eating before. I was beginning to suspect that the glucola drink was just a lot more sugar than my body is used to processing in on sitting and the results just my bodies way of saying, “WTF!! Don’t do that!!” I’ll be curious what my doctor/dietician say after reviewing my first week logs, but definitely feeling more optimistic after reading your post. Thank you♥️
Yeah, I’m 28+6. I had both 1-hr & 3-Hr Glucose Tolerance Tests. Failed both. I’m watching my carbs per the dietician. Checking my glucose 4x/Day. All my readings are normal.
Thank you for this article. So inspiring and packed with very interesting information! I’ve decided to skip the glucola test now that I’m 10 weeks pregnant and monitor my glucose at home. I find it much more interesting to know better my body and food choices. I eat low carb but increasing a bit my carb intake during pregnancy… some legumes, some fruits…but I have some doubts so yesterday I bought your book, it will arrive sometime this week…and I’m impatient to read it! 🙂
THANK YOU for this! I have been freaking out because I failed the first glucola screening and it’s 3 days later and I STILL feel HORRIBLE from drinking that “poison”! I absolutely REFUSE to do the next test they are trying to force me to do. I guess I’ll have to somehow do home screening to make sure I’m ok, but I wish I never ingested that stuff! I only eat health foods and rarely have sugars that aren’t natural so I almost feel like they GAVE me gestational diabetes! I’m still dizzy, sickly, anxiety, shaky, headache – 3 days later and I didn’t feel any of this before that horrific sugar poison drink! I’m scared it wrecked my body. But I’m So thankful for your story & glad I found your website. <3
I have a question. I had gestational diabetes in my first pregnancy. And somehow I passed the one-hourI test with my second pregnancy. I was 24 weeks and a few days when I took it and I got 116.
I’m still in disbelief I don’t have it and am a little worried I still could and maybe should be retested. What are your thoughts? My doctor said I didn’t have to do any more tests but it seems kind of wild to me that I just don’t have it again since it’s very likely to have it in subsequent pregnancies.
Thank you!
I failed the 1 hr with a 146. Been doing finger sticks 4x daily and staying under 100 with my regular diet. Mind you, I was told I still need to do the 3 hr test even though I had bariatric surgery almost 6 years ago and that much sugar in one sitting will put me down hard. The 1 hr alone almost beat me. Nah…. I’ll pass on the 3 hr and keep monitoring at home.
Please show your care team this research. The oral glucose tolerance test is not typically well-tolerated after bariatric surgery. https://www.mdpi.com/2072-6643/10/10/1479
What are your thoughts on reactive hypoglycemia during a t 3-hour test. Both myself and my sister failed the 3-hour tests but experienced pretty significant blood sugar crashes during and after the test. I generally eat very low carb diet, but increased a bit during pregnancy – not to the level that I would say the average American woman hits, but more than my norm.
Her results were higher than mine:
Fasting: 84
1- hour: 215
2-hour: 185
3-hour: 46!
(Of note, this was her only GDM diagnosis in 4 pregnancies and it was #3 and the only girl…)
My results:
Fasting: 82
1-hour: 188
2-hour: 168
3-hour: 63
Then I felt like garbage and ended up retesting with a glucometer at around 4-hours: 56!
Both diagnosed with GDM. I asked the endocrinologist about the hypoglycemia and she just said that it can happen with diabetes and more commonly with high insulin resistance.
I’d love your insight on these results.
Curious to understand your take on what I’m experiencing, or if I’m not understanding things correctly. I failed the 1 hour test by 1. I eat mainly meat and dairy with low carbs and chose to monitor my blood sugar at home. One of my readings was over 200 after one hour from eating a high carb meal with more sugar than normal in a quantity far over my daily consumption of calories as well – my husband and I were out celebrating Valentine’s Day and got really carried away (never doing this again until baby is born, lesson learned and we majorly screwed up by not adhering to our typical diet and ended upeating 300 g carbs and just under 100 g sugar).
If I understand correctly, you’re saying any reading over 200 confirms GD, but is not necessarily 100% verifiable by finger stick alone (which was how I was monitoring) unless I were to have gone in and have blood drawn? I was told the amount of carbs and sugar don’t determine how high your blood sugar could jump to and I have GD based on the one high blood sugar spike in addition to the failed 1 hr test regardless of the rest of my blood sugar readings.
When I mentioned how reducing carb and sugar intake can lower blood sugar (and the counselor agreed this impacts blood sugar levels) and asked if that could potentially impact why I had that one crazy spike and the rest of the normal readings instead of a GD diagnosis (again, huge abnormal amount of carbs and sugar), I was told whether I ate 50g of carbs/sugar or 100g of either, my blood sugar would still be that high, period. This contradicted what we both agreed with how lowering the amount of carbs consumed can lower blood suagr. My fasting blood sugar has been between 70-80, with the average being about 78 for fasting, and my blood sugar levels didn’t break over 100 by eating what I normally eat. I’m told I shouldn’t be asking these questions and just accept that I have major GD issues. I’m led to believe that had we not gotten carried away with that one meal, or had I been untruthful and just recorded something in the typical range I was given and lied, I wouldn’t have been so readily diagnosed.
I was told I could try the 3 hour test and it was bragged up to be super accurate, even with my current low carb diet. I disagreed and said I was skeptical given my low carb diet and how my body isn’t processing large amounts of carbs and sugars like I would be given. This is also something I believe you touch on with the 3 hour test not being as accurate as commonly believed – please correct me if I’m wrong.
I understand you can’t give medical advice here, but I am hoping you could shed some light on things and help me understand what I’m being told. The logic I was told about the amount of carbs and sugar ingested seems contradictory to me and is not making sense the way the counselor described the logic to me. I was told I shouldn’t be asking questions and to just accept my diagnosis as is after attempting to get clarification on how the diagnosis was reached in two separate discussions. I clearly explained I was looking to understand why the one data point would lead to that diagnosis when the rest of my levels have been prefectly fine and that I had questions I wanted answers to and that the discussion was not to get the GD diagnosis changed. I was also told I should be eating 170 g of carbs daily, which became more of the diabetic counselor’s concern than attempting to address my questions and provide any evidence into her decision other than that’s what she decided.
Regardless, I intend to speak with my OB at the next appointment and hope she can answer some of my questions. I haven’t strayed from eating my normal low carb diet which has been giving me low, normal readings like the meals before and the fasting blood sugar level the day after the big mess up meal, and I intend to keep it that way for the rest of the pregnancy.
Thanks!
I recently failed my 1 hour test with a score of 180. Before taking the test I had forgotten that I was scheduled for it the day I went in for my visit. I did not get a chance to eat in the morning so I stopped at smoothy king and got a strawberry, banana and peanut butter smoothie. I drank a lot of it before going in for my visit. I asked if this would effect my results and if I should just come back the next day and they said is wouldn’t.
With my 1st child I was borderline with a score of 142 so I retested with the 3 hour test and “passed”. This time around my doctor was out of the country when my results came in and they did not get back to me with results for almost 2 weeks. To say I was extremely unhappy is an understatement. The nurse on the phone did not even offer me the 3 hr. test. This concerned me. I started the finger sticks and made an appt. with the nutritionist.
I will admit I was afraid to eat carbs after hearing the results. I did not cut them out completely but I just stayed away from bread, pasta and rice. In all honesty I do not eat these much normally. Testing at home my numbers were all low. By the time I spoke with the nutritionist she said I could keep testing at home or take the 3 hr. I decided to test at home. She said eat the way I would normally eat without changing my diet and monitor my results. Based on the results I had from those days she didn’t seem to think I had GD but needed more data to rule it out.
It has been 10 days and I have tested >140 1 hr. after every meal and my fasting average is in the 70’s. It was my birthday during this time and I went all out just to see how I would react by having pizza and ice cream cake, my level was at 108 after an hour.
Please note I am not a sweets person. I have them on occasion but typically I prefer fruits. I do eat bread, pasta and rice but not all the time. I am wondering If because I do not eat heavy carbs often if this is why my glucose 1 hr test was so poor. Any thoughts as to why I would fail that so miserably but after testing at home my number are well below what they tell me they should be?
Thank you for your blog it has made me feel a lot better about things.
Hi Lily,
I have heard your talks about the Stanford studies that mildly elevated levels in early pregnancy cause issues with development. If these tests mess with our glucose, and in my case left me slightly higher the rest of the day – aren’t I just putting my child at greater risk with these tests?
thanks,
Jessica
I can understand that concern (and there are other options than the glucola, outlined in quite a bit of detail in Ch 9 of Real Food for Pregnancy). The issue with skipping any gestational diabetes screening (glucola or otherwise) is that if left undiagnosed, there is a risk of ongoing elevated blood sugar for the remainder of pregnancy, which has clear and documented negative effects on both mom and baby. A few hours of dysregulated blood sugar from the glucola (glucose tolerance test) is less of a risk than months of uncontrolled blood sugar. But again, there are alternatives for those who don’t want to partake in that particular test; whether or not your provider is open to those alternatives is another story.