Pregnancy puts many organs and systems in your body to the test and that includes your thyroid. If you’re not yet acquainted with this tiny little gland, your thyroid is located at the front of your neck and produces several hormones that are crucial to maintaining your metabolism as well as co-regulating other hormonal systems in the body.
During pregnancy, your thyroid gland must ramp up production of hormones by more than 50%. This is not only for your body, but because your thyroid hormones are transferred across the placenta throughout pregnancy where they play an essential role in development, particularly for brain development of your baby.
Up until mid-pregnancy, your baby is entirely reliant on your thyroid hormones (it’s only around week 16-20 that the fetal thyroid gland is mature enough to produce its own hormones). (Neuroscience, 2017)
This is all well and good until the thyroid has trouble keeping up with the increased demands of pregnancy. Sadly, this scenario is incredibly common.
The importance of identifying and treating thyroid problems cannot be understated and an underactive thyroid, called hypothyroidism, is the most common manifestation.
As such, this article will primarily focus on hypothyroidism and pregnancy.
Why Thyroid Health Matters in Pregnancy
There are numerous ways that your thyroid health can affect you and your baby during pregnancy.
As one study points out, “hypothyroidism may be associated with miscarriages, low birth weight, anemia, pregnancy-induced hypertension, preeclampsia, abruption placenta, postpartum hemorrhage, congenital circulation defects, fetal distress, preterm delivery, and poor vision development, in addition to the probable neuropsychological defect in the child.” (Diseases, 2016)
Your baby’s brain development is highly dependent on your thyroid hormone levels. Mild to moderate thyroid dysfunction can result in neurodevelopmental problems ranging from low intelligence, delayed verbal development, impaired motor performance, autism, and attention-deficit hyperactivity disorder (ADHD). (Neuroscience, 2017)
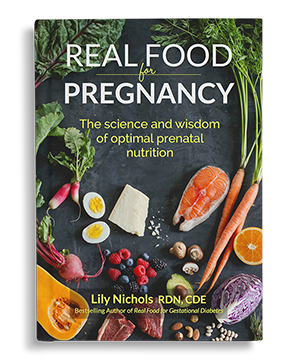
If that sounds rather serious, it is! When I was researching and writing the section on thyroid health for Real Food for Pregnancy, it was astounding to see how much solid research is out there on this topic. It’s truly a wonder why thyroid health in pregnancy isn’t discussed more often.
How do I know if my thyroid is adapting to pregnancy?
The only way to know if your thyroid is functioning well is to get blood work run. Unfortunately, this is not routinely run in most medical practices.
Many endocrinologists have been pushing for universal thyroid screening in pregnancy, but it has yet to be widely adopted. At the very least, the American Thyroid Association recommends routine screening for anyone with the following risk factors: (Thyroid, 2017)
- over the age of 30
- history of miscarriage, pregnancy loss, or infertility
- preterm delivery with a prior pregnancy
- autoimmune disease
- obesity
- family history of thyroid problems
- people who reside in an area where iodine deficiency is common.
The ideal time to get your thyroid tested is actually preconception, so you can take steps to optimize your thyroid function before you conceive. That’s because the increased demands on your thyroid start early on in pregnancy, possibly before you even know you are pregnant. That means your window to correct hypothyroidism is rather slim.
In one study, the rate of fetal loss was 60% in women with overt, untreated hypothyroidism. (Thyroid, 2002) If you have a history of miscarriage, it’s even more important to have your thyroid checked.
If you’re already pregnant, don’t fret. Simply ask to have a complete thyroid panel added to your first trimester blood work.
A complete thyroid panel in pregnancy typically includes the following labs:
- Thyroid Stimulating Hormone (TSH)
- Free T4
- Free T3
- Reverse T3
- Thyroid Peroxidase Antibodies (TPOAb)
- Thyroglobulin Antibodies (TgAb)
Keep in mind that many practitioners only order TSH and maybe T4, so you’ll need to push for a full panel. I’m especially partial to getting a full panel to help identify if there are elevated thyroid antibodies.
That’s because high antibodies during pregnancy are significantly linked to the development of thyroid issues postpartum. Researchers note that the “vast majority of women who develop postpartum thyroiditis are thyroid antibody positive prior to pregnancy.” (Frontiers in Endocrinology, 2015)
In other words, these women already had signs of autoimmune thyroid disease before having a baby, and the stresses incurred on the thyroid during and after pregnancy triggered full-blown thyroid disease.
It’s estimated that 10-17% of women have thyroid autoimmune disease during pregnancy (meaning they are positive for thyroid antibodies but have otherwise normal thyroid hormone levels). In these women, fully one third will develop postpartum thyroid problems within the first year after delivery. (Frontiers in Endocrinology, 2017)
If your provider is resistant to testing a full panel, feel free to share the above research with them.
Will I have symptoms if my thyroid is off?
Maybe, but not always. Fully 70% of women with hypothyroidism have no obvious symptoms. (Fertility & Sterility, 2015)
According to some research, lack of nausea or morning sickness in the first trimester can be a sign of underactive thyroid and/or iodine deficiency. (Journal of Theoretical Biology, 2014)
Depending on whether you’re hypothyroid or hyperthyroid, the possible spectrum of symptoms can vary.
Feeling too cold or too hot, easily fatigued, lack of change in appetite, anxiety, irritability, depression, tremor, rapid heart rate or palpitations, dry skin, and difficulty concentrating can be (but, are not always) related to thyroid issues.
What if I already know I have a thyroid condition?
This is when it’s crucial to have an experienced care provider who’s familiar with the complex adaptations that the thyroid makes during pregnancy (and the trimester-specific reference ranges that complicate interpreting those labs).
This is precisely why I do not get involved in arguing for/against certain ranges of thyroid hormones in pregnancy. It’s complicated and clearly outside of the scope of practice as a prenatal dietitian. Again, defer to your care provider for guidance. The purpose of this article is to help you understand the role of your thyroid health during pregnancy and what to ask for so you can get the proper screening; not to give clinical guidance.
If you’re taking replacement thyroid hormone already, your dosage will likely need to be adjusted (usually up) to account for that 50% increase in demand. Testing your thyroid hormone levels often can help with this. Clearly, this is something you need to work with directly with your provider.
First-hand accounts on managing thyroid conditions during pregnancy
I recently did an interview with Allie Hobson of the Nutrition-ish podcast. She has Hashimoto’s, which is a form of autoimmune hypothyroidism (that’s extremely common in women, by the way).
In our interview, she shared a detailed account of how she needed to adjust her thyroid medication based on her lab tests (and advocate for even more frequent lab tests than her provider initially recommended).
Tune into Episode 37 of the Nutrition-ish Podcast to hear our full conversation. The thyroid part of our talk was about halfway through.
I was humbled to hear that she used my book, Real Food for Pregnancy, to guide her during pregnancy, including helping her understand how her Hashimoto’s would likely be affected. This helped her plan for getting her thyroid labs tested often and made her realize that it was entirely normal for her thyroid medication dosage to increase quite a bit.
As a result, she’s been able to keep her thyroid hormone levels in a healthy range during her pregnancy (woohoo!).
In addition to talking about thyroid health in pregnancy during our interview, we take a deep dive into a variety of nutrition topics.
Here’s an overview of our interview:
- Our frustrations with condescending prenatal nutrition advice.
- Why I think telling pregnant women to “do your own research” isn’t fair (shouldn’t the guidelines reflect the research in the first place?).
- Preconception – how soon before you try to conceive should you and your partner work on your diet and lifestyle.
- The nutritional trade off of strictly adhering to conventional “foods to avoid” lists and a deep dive into a discussion on undercooked eggs, salad greens, raw dairy, raw fish, deli meat, and jerky.
- Allie’s journey with managing Hashimoto’s thyroid disease (an autoimmune hypothyroid condition) during pregnancy. She shares about how she pushed for extra thyroid testing and aggressive dosage adjustments to her thyroid replacement hormone therapy to keep her thyroid hormone levels in check.
- How thyroid metabolism changes during pregnancy and why it plays a role in your baby’s brain development.
- Nutrients and their food sources that support thyroid health during pregnancy.
- Should you eat certain foods during pregnancy with the goal of reducing your baby’s chances of allergies?
- Testing for gestational diabetes: Arguments for or against the glucose tolerance test (glucola) commonly used to screen for gestational diabetes (more on this topic here). Is the jelly bean test, juice, or a test meal accurate? What about home blood sugar monitoring?
- My thoughts on how to support digestive function during pregnancy.
To listen to our full interview, listen HERE or on iTunes (Nutrition-ish Podcast, Episode 37).
Keep an eye on thyroid function postpartum
Before you go, I want to give a little PSA on thyroid function postpartum (or perhaps I should say thyroid dysfunction postpartum!).
As your body readjusts after birth, hormone levels can take some time to find their equilibrium. Often, the focus is just on female hormones, but your thyroid gland—and all of its hormones—must also find a new normal. Sometimes this process is relatively uneventful, and other times, thyroid problems develop.
Thyroid abnormalities that appear within a year of giving birth, collectively known as “postpartum thyroiditis,” are surprisingly common. In fact, “up to 23% of all new mothers experiences thyroid dysfunction postpartum, compared with a prevalence of 3-4% in the general population.” (Frontiers in Endocrinology, 2017)
That means almost a quarter of new moms have a thyroid issue.
Having a properly functioning thyroid is important for maintaining your energy levels (obviously necessary when trying to keep up with a baby or toddler), supporting your fertility (if you want another child, this is crucial), promoting normal postpartum weight loss, and for your mental health. Postpartum thyroid dysfunction is a known risk factor for postpartum depression. Simply put, your thyroid function is a quality of life issue.
Obviously, I’m a strong proponent of having your thyroid tested—preconception, during pregnancy, and postpartum!
If you ever wondered why thyroid health matters in pregnancy, hopefully this article has given you a little clarity around the crucial role that this tiny little gland plays.
If you have any experience with thyroid conditions in pregnancy, feel free to share them in the comments. We can all learn from each other’s experiences here.
Until next week,
Lily
PS – For more on how the thyroid adapts to pregnancy, see Chapters 9 and 12 of Real Food for Pregnancy. Also, see Chapter 10 for information on how to minimize exposure to specific toxins that can interfere with thyroid function (there are many and the research is all clearly documented if you want to dig deeper). This post includes multiple excerpts from the book, so if you like this style of writing and the emphasis on in-depth, evidence-based information, chances are you’ll want a copy of the full book. Take a sneak peek for free by downloading the first chapter below.



I gave birth on November 7, 2018 and my thyroid started acting up immediately after. My heart rate was jumping to 120 from just standing up and you could visibly see how fast my HR was from looking at my chest. I would also feel pretty light headed standing for too long. My thyroid was tested the following day and showed I had an abnormal hypothyroid, but was having symptoms of a hyperthyroid. I’m still waiting for my appointment with an endocrinologist, but in the meantime my midwives retested my thyroid while I was on 50mcg of Levothyroxine after a week. The results came back that my thyroid was back to normal levels. I will continue with this medication until I meet with an endocrinologist in January. I had no idea this was so common and would’ve loved to know more sooner! I wonder if my thyroid was off while I was pregnant..
It’s very common to have postpartum changes to the thyroid. As I discuss in chapter 12 of Real Food for Pregnancy, sometimes the thyroid shows a “triphasic pattern” where your labs can show hyper-, hypo-, and normal thyroid function in the year or so postpartum. Really helpful to follow up with your provider, especially if you’re symptomatic. I’m glad you spoke up and got proper labs done right away. Good for you!
I can speak from personal experience after having multiple miscarriages how important it is to get your thyroid checked. I only wish I would have known this information when we started our TTC journey to have a baby.
We did eventually stop having miscarriages (my daughter is now 8 months old), but only after correcting my hypothyroidism. I then had a reproductive endocrinologist on my team to help adjust my medication throughout pregnancy and now follow up with her postpartum to keep an eye on things.
I’ll be sharing this article, so I can hopefully help other women from having fertility struggles from thyroid conditions like me. I’m just so grateful to have finally figured it out and to have been able to sustain a pregnancy with normal thyroid levels.
I’m so sorry to hear of your losses. Glad to hear you got expert help in identifying and treating your hypothyroidism in pregnancy and ultimately were able to have a healthy baby girl. <3
I don’t know why this information on thyroid health in pregnancy isn’t more widely discussed! Those stats you gave on miscarriage related to thyroid conditions is crazy high. Thank you for writing this.
*Off to schedule a call with my doctor to run a complete thyroid panel. Fingers crossed it comes back normal.
I agree, thyroid health in pregnancy needs to be discussed more often or openly! Glad you’re getting your thyroid tested.
I was diagnosed with Hashimoto’s as a young woman (several years before my first pregnancy). I am now days away from giving birth to my second child, and what has struck me is how differently my thyroid health fared in each pregnancy. With my firstborn, my medication was continually reduced to less than half of my pre-pregnancy dose, whereas my dose was increased by about 25% in this pregnancy. This highlights the need for regular thyroid monitoring during each pregnancy—don’t assume that each one will be the same!
Absolutely can be so different pregnancy to pregnancy. Thanks for sharing your experience!
This article has been a reflection of all my worst fears coming true.
I have had Hypothyroidism since birth and feel that I manage it well but have always been afraid of having children and the effects it might have on them.
After recently becoming pregnant I have been insistent to my doctors on monitoring my thyroid and feel that it has not been given proper attention as my thyroid levels are still low, I’m on the 13th week of my pregnancy and there have been no adjustments made to my dosage. Despite my asking if there should be.
After reading the insanely triggering list of side effects I am at a loss as whether to be upset with myself of my doctors for telling me everything will be fine.
I appreciate that this article is spreading awareness for mothers to be as it is a very serious issue that medical professionals should be discussing and managing at a higher standard.
As someone who has had this condition their entire life I have been actively seeking information on my condition endlessly, to think that this is the first I’m learning about the side effects during pregnancy is very confronting and upsetting. Especially that no doctors have taken the time to discuss this with me throughout the last couple of months to get ahead of what could end up being a heart breaking situation.
Thank you to for your contribution to the awareness of expectant mothers.
I became hypothyroid when I went off of birth control. It took a lot of research and finding the right endocrinologist (paying out of pocket) to finally be properly diagnosed and treated. I have trouble converting T4 to T3 so need to be on natural dessicated thyroid (NDT) which contains both. My first OB warned me that I would miscarry if I took anything other than Levothyroxine. Scary, but I trusted my endocrinologist who monitored my thyroid panels and adjusted my NDT throughout my (healthy) pregnancy and after. I have plenty of energy and feel great on the NDT. I really wish more doctors were better educated in this area and took female patients’ complaints of fatigue and related synptoms more seriously. There are amazing endocrinologists out there but they are hard to find and you have to be lucky enough to have one in your area. Women deserve better.
I had never had any thyroid issues in my life until my current pregnancy. I had a full thyroid panel during and after each of my previous pregnancies and they both came back normal-and within the normal range for pregnancy specifically, which is of course lower than usual. And so with knowing what I know about the importance of normal TSH during pregnancy, I was especially alarmed to test as late as my 12th week of pregnancy to find I had elevated levels (5.99), this was considered subclinical and not overt hypothyroidism. What was even more alarming is that my OB told me he wasn’t concerned considering the ACOG doesn’t even recommend running a thyroid panel during pregnancy. I got second and third opinions from other doctors and while they suggested seeing an endocrinologist, they similarly shared a lack of concern for my baby’s health. I finally got put on medication after seeing an endocrinologist, but even she does not seemed concerned about my baby’s brain. All medication prescribed was done so solely to mitigate any symptoms I might be experiencing-symptoms that, mind you, are similar to general pregnancy symptoms and I couldn’t care less about relative to my baby’s development. While their lack of concern is somewhat a comfort, I can’t help but feel worried about the long term implications for my baby. I guess only time will tell.
Is there a website that you can recommend that would specificy which levels are normal ranges during each trimester?
Hi..I just wanted to share my hypothyroid and pregnancy experience …I’ll bullet point in.place to keep it short.
2019 out of the blue developed erratic cycles, no energy..didn’t feel like myself.
Back and fourth to my doctor and was told it’s just the onset of perimenapaus..
Sept 2020 my hair fell out in huge patches, we were also trying for out last baby since 2019..it wasn’t happening.
Feb 2021 Gynacologist said i had premiture overian failure and most likely Hoshimotos hypothyroid. I was refered to an Endocrinologist who put me on 50 then 75mg of levnothyeroxine and said i was on it for life.
January 2022 found I was pregnant, OVERJOYED!!. Could not get an appointment with Endocrinologist so put my self up on 100mg in anticipation of seeing my Endo and knowing my dose must go up. I called my endocrinologist clinic informed her team of my situation and needed an appointment asap!. I also had full thyroid panel while waiting to see endo…she never got back to me.
I missedcarried my baby at 13wks at home naturally having been told my baby’s heart had stopped at 9 weeks.
ANGRY AND DEVISTATED.
I got an appointment from my endocrinologist after the fact for April 2022…too little to late!.
Now, No history of thyroid problems or hairloss in my family..ever.
1.I was never told if I was primary, 2nd, temp But perhaps Hashi.
2,I asked if there was somthing I could do with my diet to help / supplements ect. I was told No.
3.I felt abandoned by my endo and lost my baby.
I have been researching like crazy about Hashi thyroid and have learned it Can Be Reversed(side note, I’m health conscious, eat low carb ,keto , don’t smoke ect)
So, New plan , I’m weaning myself off levnothyeroxine, While supplementing with Iodine, Selenium, zinc, D3&K2,Clonfolic and macc root And a daily massage of frankensene essential oil on my thyroid and my feet…and if my Husband is willing..to try for our last baby ( lucky number 4) .Im 43, I refuse to pop a pill that will eventually kill my thyroid anyway and be told that’s it..
There has to be a better way.
Whish me luck!
Hey Lily, I’m interested to hear your thoughts on treating impending autoimmune hypothyroidism with a gluten-free diet. Prior to conception I had a complete thyroid panel which showed elevated thyroid antibodies, but normal thyroid hormone levels. My functional medicine doctor recommended me going gluten-free (even though I don’t have celiac disease or gluten sensitivity). The idea is based off of molecular mimicry. Anyways, I wanted to get your thoughts on this because I’m okay with going 95%gluten free, eating a whole food nutrient dense diet, but so far doing a literature review, I haven’t come across any evidence for going 100% gluten-free. Thanks in advance!
Did you have any luck with this Carrie? I am in the same boat with TPO antibodies about 200 but my TSH is normal. My levels were monitored in my first pregnancy and were normal throughout with only T3/T4 can’t remember which being borderline low but my OBGYN said that didn’t warrant going on medication since TSH was normal. What was your experience?
I’ve untreated hypothyroidism. Normally the tsh level is 6.3 but when I got pregnant it went down to 1.4 I don’t know what to make of this?