In a society where a lot of emphasis is placed on a woman’s looks and appearances, it’s no wonder that weight gain during pregnancy is such a touchy subject.
Prenatal weight gain may be one of the most (if not THE MOST) sensitive topics around pregnancy, so much so that some prenatal healthcare providers don’t take the time to talk about it, leaving many in the dark about how much weight gain is right for them.
On the other hand, if weight gain recommendations are shared, they’re not always shared in a supportive way (size and weight shaming is real, my friends) and do not necessarily come with advice about how to achieve those goals (i.e. no discussion of lifestyle choices that support gaining within a certain range).
A 2018 review of 54 studies on “weight communication” in prenatal healthcare found that a discussion of prenatal weight gain did NOT happen for the majority of pregnant clients. It’s highly variable with studies reporting a range of anywhere from 9.5% to upwards of 83% of pregnant clients reporting having had this discussion. Moreover, when it was discussed, the weight goals given were inconsistent and not necessarily evidence-based. Oy!
So, I think it’s time to talk about pregnancy weight gain and in a nuanced, non-judgemental way. This post will cover pregnancy weight gain guidelines, whether research supports such ranges, and when/how it makes sense to discuss weight gain (if at all) during pregnancy.
Does weight gain in pregnancy matter?
Yes and no.
Pregnancy weight gain can be a proxy of whether or not a woman is getting adequate nourishment for both her body and baby’s growth. I say “can be” because weight alone is not necessarily a perfect indicator of anything; it’s simply one of many data points that can help you and your provider assess where you’re at.
For example, in years past (and to this day, in some communities with food scarcity), inadequate weight gain was the major concern for pregnant mothers. It can be an indication of insufficient energy intake (coupled with inadequate micronutrient intake) to support baby’s optimal growth, particularly brain development.
Inadequate weight gain can also be a surrogate marker for severity of preexisting health markers. For example, among women with inflammatory bowel disease (such as ulcerative colitis and Chron’s disease), inadequate weight gain is associated with intrauterine growth restriction and preterm birth, likely a result of preexisting inflammation and or inadequate nutrient intake/absorption.
Nowadays, in most developed countries, the concern has shifted to higher-than-expected weight gain in many situations. In one study of nearly 30,000 U.S. mothers, 51% gained above recommended weight gain, while only 21% gained below the guidelines (more on those guidelines below).
Over-consumption of processed foods, like sugar and white flour, can be (though is not always) a predisposing factor in excessive weight gain. The shift on the scale, in this scenario, is simply a reflection of the quality of the diet. A dietary pattern with lots of “empty calories” (especially sugar) and the resulting weight gain can predispose a mother to complications such as gestational diabetes or preeclampsia.
There are, of course, other scenarios where weight gain that some would call “excessive” or “inadequate” is precisely what that woman’s body requires. In the case of a woman who is consciously eating a nutrient-dense diet and following her hunger-fullness cues, her body may choose to gain in a pattern different from the chart in her providers’ office and that’s not necessarily a problem. Follow me? If she’s already doing everything within her control to nourish and care for herself, then her unique pattern of weight gain is normal for her.
Those charts are based on statistical averages and therefore there will always be “outliers” that don’t fit the mold exactly. This isn’t necessarily a bad thing! We aren’t robots.
It’s nourishment that matters, not necessarily the number on the scale.
But, I get it. You’re here to get guidance on how much weight to gain during pregnancy and have a better gauge of what counts as “too little” or “too much.”
Some find comfort in knowing how much weight they can expect to gain during pregnancy, so your mind can be at ease when your body is changing so rapidly.
This is a surprisingly nuanced discussion because it depends on many factors. Context is important here.
UPDATE: Since I first wrote this article, many practitioners reached out to have a deeper understanding of pregnancy weight gain guidelines and strategies for navigating discussions around weight gain in pregnancy. For a deep dive that goes beyond the information in this blog, check out my 2-hour webinar on Weight Gain in Pregnancy via the Women’s Health Nutrition Academy.
Pregnancy weight gain: there is no such thing as “one size fits all”
Before we go into recommendations, it’s important to understand there is no “one size fits all” recommended amount of weight to gain during pregnancy.
There are guidelines around healthy weight gain ranges based on your height-to-weight ratio—aka your BMI (body mass index) — though even these vary from country to country.
The elephant in the room: BMI
BMI is not a perfect measure of health, but it’s the most convenient measure we have in healthcare to get a rough assessment of body proportions. Unfortunately, there are some with a “high” BMI that are told they weigh “too much” when in fact their body composition is simply on the muscular side. On the other hand, a person who falls into the “normal” BMI category may actually have non-ideal body composition, with low muscle mass and lots of visceral fat (fat around the organs).
In other words, BMI is not always a reflection of your metabolic health. For this reason, I believe BMI should be used cautiously.
It would be really nice if, instead, we had widely available measures for body composition, such as bioelectrical impedance analysis (BIA), but the equipment is expensive (therefore inaccessible in most practices) and setting reference ranges for pregnancy is a huge challenge given the higher fluid levels during pregnancy and the fact that these fluid levels are ever-changing in different stages of pregnancy.
Suffice to say, what would be ideal is not always practical and hence we have the imperfect measure of BMI to guide weight gain guidelines in pregnancy.
With all of those disclaimers out of the way, weight gain recommendations are set based on BMI categories and despite the limitations, there is pretty good evidence to support different weight gain recommendations for different BMI categories.
I discuss this in more nuanced detail in this video, which I recorded on Instagram Live to answer audience questions about prenatal weight gain.
Pregnancy Weight Gain: How much can I expect to gain and does it matter?
How much weight “should” I gain during pregnancy?
Like many things in prenatal nutrition, “should” is a bit of a trigger word.
The “ideal” amount of weight to gain during pregnancy — if there is such a thing — remains up for debate.
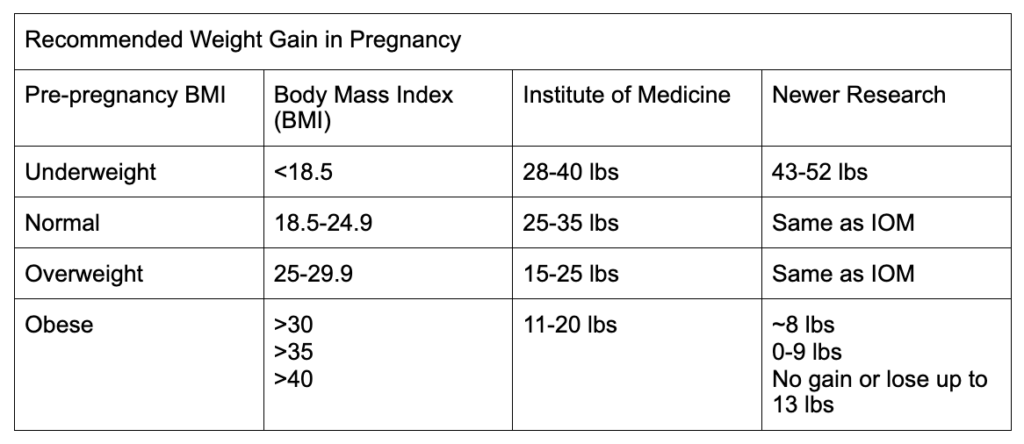
The following table shows you the Institute of Medicine recommendations, which are the most widely used standard in the United States as well as many other countries. In the column on the far right, you’ll see there’s some new research that has brought those ranges into question, particularly for women with BMI <18.5 and over 30. I discuss this research in the video included above (full citation list at the bottom of this article).
Note that BMI should always be calculated with prepregnancy body weight.
UPDATE: Since I first posted this article and generated this table, additional research has come out questioning IOM weight gain ranges for pregnancy. This data is covered in my 2-hour practitioner webinar on Weight Gain in Pregnancy: An Evidence-Based Analysis via the Women’s Health Nutrition Academy. I also cover the latest research on weight gain for twin pregnancy and weight gain for triplet pregnancy.
Something that often gets lost in discussion of recommendations is why the body naturally gains weight during pregnancy.
Here’s where the extra pounds go. These are approximate estimates for a woman with a BMI in the healthy range preconception; these will naturally vary woman to woman:
- Baby: ~7.5 pounds
- Placenta: 1.5 pounds
- Breast tissue (to get ready for breastfeeding): 2 pounds
- Increased fluid volume: 4 pounds
- Increased blood volume: 4 pounds
- Uterus: 2 pounds
- Placenta: 2 pounds
- Maternal fat stores: 7 pounds
If you add all these up, we are looking at around 30 pounds.
So, if you’re worried about “all the weight I’m gaining,” rest assured that the extra pounds are there for very important reasons.
As you can see, for most women, gaining some weight is perfectly normal and HEALTHY. Again, if you haven’t watched yet, I discuss some of the nuances to this, especially for women who fall into lower or higher BMI categories in the video above.
What are the risks of gaining “too much” or “too little” weight in pregnancy?
The reason that we have weight gain guidelines in the first place is that there can be risks associated with lower or higher-than-expected weight gain, although keep in mind that there are no absolutes.
Studies have shown that gaining above the guidelines during pregnancy can increase the likelihood of adverse pregnancy outcomes for both the mother and baby, including higher rates of:
- Gestational diabetes
- Preeclampsia and gestational hypertension
- Postpartum hemorrhage
- Shoulder dystocia (shoulders get stuck during delivery)
- Macrosomia (baby is larger than expected)
- Neonatal hypoglycemia (baby’s blood sugar drops too low after birth)
Risks of too little weight gain include higher risk of:
- Preterm birth
- Low birthweight
Some of the above risks also hold true for women who start their pregnancies at either very low or very high BMIs, though they are mitigated with pregnancy weight gain within the guidelines. I’d defer to the “newer research” column in the chart above over the Institute of Medicine goals to minimize the risks.
In other words, women with a prepregnancy BMI <18.5 have fewer pregnancy complications with weight gain that is higher than the current Institute of Medicine recommendations. Women with BMI >30 (and particularly BMI >40) have fewer pregnancy complications with weight gain that is lower than the current Institute of Medicine recommendations.
UPDATE: Since I first wrote this article, many practitioners reached out to get specific data on the relative risk of these pregnancy complications based on pregnancy weight gain. If you really want to dive into the details on pregnancy weight gain data, check out my 2-hour webinar on Weight Gain in Pregnancy via the Women’s Health Nutrition Academy.
So, how do I gain the “right” amount of weight during pregnancy?
I sincerely hope that your takeaway from this article is NOT to nitpick the numbers on the scale. My hope is that this information provides you with a loose framework to set your expectations on how much weight gain is associated with optimal pregnancy outcomes for you and baby.
It comes down to this: The better you nourish yourself, the better you will nourish your growing baby.
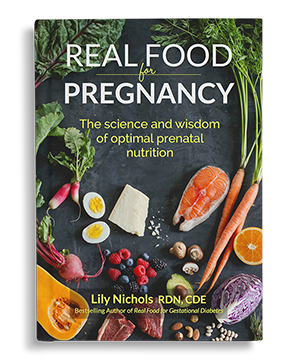
In my experience working with hundreds and hundreds of pregnant women directly and now hearing from tens of thousands who have used my books to guide their pregnancies, your body will gain the appropriate amount of weight for you given that it is provided balanced nutrition, blood sugar levels are maintained in the normal range, and some light to moderate activity is continued through pregnancy.
When it comes to nutrition, the top three things that help your body gain the right amount of weight for you are:
- Eat adequate amounts protein (see Ch 2 of Real Food for Pregnancy; research has shown we need a lot more than previously thought)
- Choose low-glycemic carbohydrates (key for blood sugar balance & studies have shown w low glycemic diet significantly lessens pregnancy weight gain)
- Eat mindfully
I can say a heck of a lot more about healthy eating in pregnancy, but that’s why I wrote books on these topics. Real Food for Pregnancy would be the best place to go for this information.
When it comes to exercise, a meta-analysis of randomized controlled trials from 2019 found that in women who exercised on average 30-45 minutes 3 days a week, there was a significantly lower risk of gaining excessive weight in pregnancy. For more on safe exercise in pregnancy, see Ch 8 of Real Food for Pregnancy.
Real women share their pregnancy weight gain stories
I’ve witnessed the power of real food in optimizing weight gain time and time again in practice and now receive emails sharing these stories on a weekly basis. The following stories are all shared with permission and anonymously.
For example, Kim contacted me to share that she had gained 75 pounds in her first pregnancy (was in the “normal BMI” category prior to pregnancy). She developed gestational diabetes and was managed with the standard dietary advice (>175g carbs per day) and insulin. She felt incredibly uncomfortable in the latter months of pregnancy with all the swelling she had and struggled to lose the weight postpartum. When she conceived her second, she was reading Real Food for Pregnancy. This pregnancy, she was starting at a BMI of 29. She ate a lower carb, low glycemic diet of real foods and gained a total of 18 pounds. She did not develop gestational diabetes, did not get swollen at the end, had no heartburn or hip pain, and lost the baby weight within 2 months postpartum. She told me how it was an entirely different pregnancy and postpartum experience as a result.
Another example for you. This one was a client of mine, so I’m not using her real name. Let’s call her Jenny. She came to me in her 3rd pregnancy. She had gestational diabetes in pregnancy #2 and managed it ok with the help of her doctor, however, she gained 45 pounds and her baby was large for gestational age (9 lb 15 oz) and had to be treated for hypoglycemia. In her 3rd pregnancy, her blood sugar was more difficult to control (this is common in subsequent pregnancies), leading her to reach out to work with me and ultimately join the Real Food for Gestational Diabetes Online Course (where I can provide participants with direct feedback during weekly office hours in our private course community). With this pregnancy, she was really hoping to stay off of medication and avoid having any complications at delivery. With dietary and lifestyle changes, she maintained excellent blood sugar control. Her total weight gain was a full 20 lbs less than the previous pregnancy and baby was 7 lb 13 oz, no hypoglycemia.
For anyone concerned about not gaining enough weight, Suzanne reached out to share her pregnancy story. She shared that her body naturally errs on the lower weight (BMI right on the lower end of normal), despite not restricting her food intake or over-exercising. She followed my dietary principles in her pregnancy, especially being cognizant to get enough protein and whole foods in her diet. Her providers were worried that she wasn’t gaining enough weight, but she watched my IG video (re-posted in this article; scroll up!) and realized she was only a few pounds below their recommendations. Plus, she’s 5’1”, so it made sense that she might not gain as much weight as a very tall woman. Seeing that weight was only one of many ways to assess the adequacy of her diet and baby’s growth, she didn’t worry. She felt well and by all of other measures, baby was doing well. This gave her peace of mind to continue eating mindfully and stop obsessing over the scale. She ended up gaining 23 lbs and baby was born full-term and a perfectly healthy size of 7 lb 15 oz.
Finally, I’ll share a story from Marizelle, who reached out to share her story via email at 2 months postpartum. She started her pregnancy at 230 pounds and was worried that she would gain too much weight during her pregnancy and develop gestational diabetes (she was borderline prediabetic prepregnancy). Her provider had explained some of the risks of excess weight gain, which had her very concerned. Luckily, she read the weight gain section in Ch 7 of Real Food for Pregnancy and incorporated the meal balancing and mindful eating tips in Ch 2 to improve her diet. Ultimately, she had a mild case of gestational diabetes which was diet-controlled. She gained a total of 3 lbs over the course of her pregnancy (this sounds low, but was appropriate for her BMI range) and baby was born at 8 lbs exactly with no complications. By 2 months postpartum, she had dropped down to 190 lbs, had a great milk supply, and felt better than she had in years (despite the sleep deprivation).
Hopefully, these stories can serve as inspiration. It shows you that the “right” amount of weight gain is different woman-to-woman. It also illustrates that none of these women had to starve themselves; their weight gain was simply the result of informed dietary/lifestyle choices.
Pregnancy is an incentive to optimize the nutrient density of your diet, meaning every bite of food that crosses your lips is packed with nutrition. The side benefit of micronutrient-forward nutrition is that your body will naturally gain an appropriate amount of weight for your frame without you having to intentionally restrict your diet.
Lastly, when it comes to talking about weight gain in pregnancy, let me offer some words of advice for my fellow healthcare practitioners…
I’ve had a lot of questions from fellow healthcare practitioners regarding prenatal weight gain, and so I thought I’d share what I consider a really great tool for use in your practice called the 5As of Healthy Pregnancy Weight Gain, which I originally came across via Health Canada.
If you use any sort of motivational interviewing in your practice, you might already be doing this, but it helps to put a name to the method.
In my opinion, the most important one on the list is to “ask.” As a practitioner, I almost never bring up weight until invited to do so. If the client is not interested in having the conversation, we don’t discuss it and instead talk about nutrition/lifestyle without associating any numbers with it. Remember: it’s about health, not necessarily weight.
Also, we need to be sensitive to the fact that an estimated 7.5% of pregnant women have eating disorders. Talking about weight gain can be triggering, so if they ask you to please not share their weight gain or discuss it, honor that. Some prefer to turn around when being weighed so they do not see the totals.
The 5As of pregnancy weight gain are:
- Ask—for permission to discuss weight (ask Qs before making assumptions/statements)
- Assess—potential root causes of discordant weight gain
- Advise—on pregnancy weight gain
- Agree—on a realistic plan
- Assist—in identifying barriers, referrals, follow up
Some key points:
- Choose your words carefully, like: “Some of my clients find comfort in discussing recommendations on weight gain in pregnancy, while others do not. Are you interested in information about weight gain during pregnancy?” OR “Are you open to discussing your thoughts about weight gain during pregnancy?”
- Keep the focus on improving health behaviors/outcomes versus focusing on the # on the scale (i.e. better blood sugar/pressure management, lower risk of having an unusually small/large baby, improved lifelong metabolic health for the baby, easier postpartum recovery, etc.)
- (This one is from me, not the 5A program…) Acknowledge that weight gain is not entirely within your control in pregnancy. Yes, you can influence it to some degree, particularly with dietary changes, but even those can be a challenge depending on your circumstances, symptoms, finances, and much more. Reiterate to your clients to trust that by prioritizing real food and using mindful eating (as outlined in Real Food for Pregnancy), they’re doing their part, even if their weight gain does not follow the expected trajectory.
For More Information on Weight Gain in Pregnancy
If you are currently pregnant, check out the Weight Gain section in Ch 7 of my book, Real Food for Pregnancy for a nuanced, non-judgemental, evidence-based discussion on prenatal weight gain.
I’ve also written a blog post on Intermittent Fasting and whether it is a good or bad idea during pregnancy, as many who are concerned with excessive weight gain consider fasting and have asked me about this topic.
If you are a practitioner, it’s essential that you know how to assess pregnancy weight gain accurately and when (or when not) to have conversations in a positive way. In my practitioner webinar on this topic, Weight Gain in Pregnancy: An Evidence-Based Analysis, you’ll learn:
- The physiological function of weight change during pregnancy
- Overview of weight gain recommendations and data that questions their ranges (for singleton, twin, and triplet pregnancies)
- Data on pregnancy outcomes relative to gestational weight gain
- Eating disorders during pregnancy
- Use of prenatal weight gain grids and other methods for assessing gestational weight gain
- Top 3 ways to support healthy pregnancy weight gain
- Counseling tips for when, how, and if discussing weight gain is appropriate with a client
- Case studies
This webinar is available on-demand for viewing at whatever time suits your schedule.
Before you go, I’d love to hear from you.
Did your prenatal healthcare provider discuss prenatal weight gain with you? Did you like the way it was discussed or not? How so?
If you’ve had more than one pregnancy, have you found that your body just puts on a certain amount of weight each time? Or did it vary pregnancy-to-pregnancy? What was your experience?
Would love to hear your comments and thoughts below!
Until next time,
Lily
P.S. For practitioners looking to educate themselves further on weight gain recommendations in pregnancy, please watch my 2-hour webinar on Weight Gain in Pregnancy for the Women’s Health Nutrition Academy here.
References
- Weeks, Ashley et al. “Inconsistent Weight Communication Among Prenatal Healthcare Providers and Patients: A Narrative Review.” Obstetrical & gynecological survey vol. 73,8 (2018): 423-432. doi:10.1097/OGX.0000000000000588
- Whitaker, Kara M., et al. “Women’s report of health care provider advice and gestational weight gain: a systematic review.” Journal of Women’s Health 30.1 (2021): 73-89.
- Bengtson, May-Bente, et al. “Inadequate gestational weight gain predicts adverse pregnancy outcomes in mothers with inflammatory bowel disease: results from a prospective US pregnancy cohort.” Digestive diseases and sciences 62.8 (2017): 2063-2069.
- Kominiarek, Michelle A., et al. “Association between gestational weight gain and perinatal outcomes.” Obstetrics and gynecology 132.4 (2018): 875.
- de Barros Gomes, Caroline, et al. “Consumption of ultra-processed foods in the third gestational trimester and increased weight gain: a Brazilian cohort study.” Public Health Nutrition: 1-9.
- Parker, Haley W., et al. “Associations between pre-pregnancy BMI, gestational weight gain, and prenatal diet quality in a national sample.” PLoS One 14.10 (2019): e0224034.
- Berlit, Sebastian, et al. “Bioelectrical impedance analysis in pregnancy: reference ranges.” in vivo 27.6 (2013): 851-854.
- “Weight Gain during Pregnancy.” Home, www.marchofdimes.org/pregnancy/weight-gain-during-pregnancy.aspx.
- Johnson, Julie, et al. “Pregnancy outcomes with weight gain above or below the 2009 Institute of Medicine guidelines.” Obstetrics and gynecology 121.5 (2013): 969.
- Xu, Huiling, et al. “Gestational weight gain and delivery outcomes: A population‐based cohort study.” Paediatric and Perinatal Epidemiology 35.1 (2021): 47-56.
- Goldstein, Rebecca F., et al. “Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis.” JAMA 317.21 (2017): 2207-2225.
- Viecceli, C., et al. “Weight gain adequacy and pregnancy outcomes in gestational diabetes: a meta‐analysis.” Obesity reviews 18.5 (2017): 567-580.
- Qarmach, Baraa, et al. “Maternal weight gain during pregnancy and outcomes for the newborn child and mother in Tulkarem and in camps: a retrospective cohort study.” The Lancet 391 (2018): S5.
- Dude, Annie M., et al. “Gestational weight gain and pregnancy outcomes among nulliparous women.” American journal of perinatology (2019).
- Gonzalez-Ballano, Isabel, et al. “Pregestational body mass index, trimester-specific weight gain and total gestational weight gain: how do they influence perinatal outcomes?.” The Journal of Maternal-Fetal & Neonatal Medicine 34.8 (2021): 1207-1214.
- Walker, Ruth, et al. “Attenuating pregnancy weight gain—what works and why: a systematic review and meta-analysis.” Nutrients 10.7 (2018): 944.
- Wang, Jianying, et al. “Impact of exercise on maternal gestational weight gain: an updated meta-analysis of randomized controlled trials.” Medicine 98.27 (2019).
- Olander, Ellinor K., Briony Hill, and Helen Skouteris. “Healthcare Professional Training Regarding Gestational Weight Gain: Recommendations and Future Directions.” Current Obesity Reports (2021): 1-9.
- Dörsam, Annica F., et al. “The impact of maternal eating disorders on dietary intake and eating patterns during pregnancy: a systematic review.” Nutrients 11.4 (2019): 840.




Lily – Thank you so much for this article. I am currently in week 33 of my 3rd pregnancy. I would consider myself a fit person both pregnant and not pregnant. However, each pregnancy, I have gained around 50 pounds. This is not because “I let myself go” or “eat for two,” but simply I think it’s what my body needs to do. Outside of pregnancy I am 5’7″ around 150 lbs and super active (I work out 5 times a week at minimum). For the past two years I have worked with a trainer who switched my thinking from weight to body composition. Before this third pregnancy, I had a BMI that hung between 21-23 and my muscle mass was over 30.2%. I have not stepped on my body composition scale since getting pregnant. In addition, in both previous pregnancies, I have had super healthy, non-complicated births that produced very healthy babies. During this third pregnancy, I really wanted to avoid gaining so much weight, so my midwife recommended your book. I read it, have been following it, and still, my body has gained more weight (55lbs) than the other two. I feel great so I’m not sure why I care so much. I know that the weight will come off, I always produce tons of milk and have had healthy babies but weight is such a shaming issue for me. I really struggle with the way my caregivers now and in the past have spoken to me about this. I understand that gaining too much weight can be a sign of more troubling things, but knowing your patient is so important. I have just felt like they only look at the number, not the composition of my body when I’m pregnant. Even though I still do cardio workouts (3x a week), some lightweight lifting, walking and yoga 5-7 times a week. I wish that I never had to be weighed at all during this time, it honestly just makes me feel bad about myself, like I’m not doing something right… even though I track everything I put into my body. Yes, we all splurge have a treat here and there, but overall I am a super healthy person, I just gain 50 pounds when I’m pregnant, no matter what. The funny thing is, I have heard this from many women. It can’t just be me, right? Thank you again for your insight on this topic, really helpful!
Absolutely not just you. It sounds like that’s the right amount of weight gain for your body. I wish more providers didn’t look at weight as the “end all be all.” Every body is different.
I really, really struggle with how to deal with my weight gain. My pregnancies have been all over the map (as have my starting weights)
1st pregnancy: started at 140, ended at 175 (gained 35 lb.)
2nd pregnancy: started at 120, ended at 180 (gained 60 lb.)
3rd pregnancy: started at 175, ended at 225 (gained 50 lb.)
4th pregnancy: started at 190, have already gained 25 lb. at week 22!
I didn’t eat sweets at all until week 20 because I did not feel well. I ate carbs from fruits and whole grains and dairy, but no desserts and tried to limit refined grains. I eat plenty of protein (120 g or more). Once I started to feel well again, I started allowing myself “treats” from time to time. Ice cream or dark chocolate usually.
I have read your books and try to apply them but I really feel much better and more energized when I am eating enough carbs. It’s been such a frustrating few years as I try to lose weight by cutting carbs, fasting, exercising more, etc., but then I add carbs back in and stop fasting and reduce exercise to deal with fatigue and low energy. I honestly don’t know what approach to take to lose weight after this baby is born. It’s very discouraging. If anyone has insight for me, I’d love to hear it.
I guess I’m coming from the opposite angle than most. In my first pregnancy (hospital birth) my midwife warned me about my 35 lb weight gain. My home birth midwife in my second and third pregnancies didn’t see my 50 and 60 pound weight gains as any cause for concern. I actually want MORE guidance from my midwife this time around as I feel I am gaining several pounds a week while trying to walk several times a week, do yoga several times a week, sleep enough, keep stress as low as possible, eat well. I know a lot of people cut out grains but I think my energy would drop again.
My midwife didn’t bring up weight gain until I asked her about it. She seemed to be very cognizant of the fact that many women have an unhealthy relationship with the scale and discouraged me from thinking about gain too much, and ultimately responded saying that she’d love if all her clients gained an average of half a pound a week. She finished by saying she’ll never bring up weight gain unless the gain seems that be related to preeclampsia/fluid overload.
I ended up gaining 45lbs with my first pregnancy. I was gaining a reasonable amount each week until the second half of the third trimester. After that: 1-I let my diet go a bit and indulged more frequently, 2- it seemed like my body was storing up all excess calories as body fat for later. I ended up with a cesarian and had no appetite until about 3 days pp. I was glad to have the extra fat stores!
Now 20 weeks pregnant and have gained 11lbs so far. I’m following many of the principles from your book (although slightly higher carb than the sample meal plans) and I think I’m on a pretty healthy weight gain trajectory!
Great article, thank you!
During my first pregnancy my BMI was just over 30. I was fit and healthy going into pregnancy and my pregnancy was perfect in every way (fundal height, blood tests and blood pressure etc), I gained a total of 5kg. At every appointment my BMI was recalculated based on my current, pregnancy weight! I felt like I was being “risked out” as the hospital’s cut off was 40- which I was never even close to. There never seemed to be any time for discussion about my other questions about labour or mothering because the focus was always on my weight, which is sad considering there was never a conversation about *what* I was eating, either! My labour was 5 hours and 15 minutes, with no tears, bleeding etc. My baby was 3.88kg and breastfed for almost 3 years. I ended up having her at home because I felt so unsupported in the hospital that I didn’t want to go in, and I knew I was very healthy and unlikely to need assistance. But I am sure there are women who would have been put in danger from that approach, your point a out *how* care providers discuss weight is bigger than it may seem at first glance. Incidentally, I declined to be weighed at all for my second pregnancy and my baby was…3.88kg at birth, same exactly as my first!
Thanks for emphasizing that providers should ask instead of assume! I am five months postpartum and during my pregnancy my midwife asked very respectfully about if weight was something I wanted to discuss, and I requested that we didn’t discuss it or track my weight at all, unless strictly necessary. I have a eating disorder history and I hadn’t stepped on a scale in years because I find it triggers obsessive thoughts for me. I like to focus on real food and intuitive eating and not the numbers on the scale. I started out at a normal healthy size and my pregnancy was normal and healthy and so there was never any need to weigh me at all, which I was super grateful for.
Such an interesting topic! I am on my first pregnancy and my weight journey has been interesting to track. I’m not sure what to make of it.
Before my pregnancy I rarely weighed myself — preferring to just go by how I was feeling, how my clothes fit, etc. Being too obsessive about weight felt unhealthy for me. But I did go to one pre-conception appointment in September and was surprised (and a little distressed) to find that I was at my highest weight ever — ~182 lbs and a BMI around 28 (I blame quarantine).
Despite hoping to get a bit more in shape before conceiving, I got pregnant very quickly after that. I did not weigh myself much those first couple months. I was quite nauseous and had lots of food aversions so my eating was not great. I was probably eating less, overall, but I was also eating very poorly (lots of simple carbs and junk food–knowing what I know now I am positive that this did not help with my nausea). But, at the same time, I got back into a better exercise routine — walking at least 3 miles a day, hiking once or twice a week, and doing some yoga and stretching.
Right around the beginning of my second trimester the morning sickness eased up and this is also when I found Real Food For Pregnancy. I began to follow the advice in the book and kept up with my exercise and started feeling really great. I switched providers at this same time and was surprised to weight in around 178 at my first appointment, which means I had LOST 4 pounds since my pre-conception appointment. Since I was eating well, exercising and feeling good and everything appeared normal and healthy with the pregnancy, I didn’t feel concerned and neither did my midwife. I did decide to track my weight more closely, however, just to get a better understanding of what my body was doing.
I am 28 weeks now and I am up to 183 pounds. I gained those 5 pounds very slowly January-April. Also, if you look at my “pre-pregnancy” weight that means I have only gained 1 pound since September. I still have a couple months to go, so I am sure I will keep gaining, but at this point I am nowhere near the 15-25 lbs suggested for someone with my BMI and I am a little doubtful I will “catch up.” Still, the baby seems to be growing well, my uterus is measuring normal, etc. So I am just guessing that eating and exercising better has caused my weight to re-distribute? My belly is definitely growing and feeling heavy so it is strange not to see the numbers on the scale going up!
Thank you for this article! I always love when you dive into new topics. The level of detail you provide is much appreciated!
I’ve had two children. Both boys are born at the exact same day in my pregnancy, were almost identical in weight/length, and I gained 33 and 32 pounds, respectively. This was very interesting to me. I read (and loved) your book while pregnant the first time and ate a balanced diet with occasional treats. With my second pregnancy, we’d fine tuned the dietary protocol for my pre-existing condition and I ate a fully real food, modified paleo diet. I thought I’d weigh significantly less than the first time but ended up with just a pound less of weight gain. That second pregnancy, I was also much more active than the first, given the fact that I had a toddler to chase. Clearly, my body knows what it needs to do to grow a healthy little one.
Interestingly, my midwives had me eat more at the end of my first pregnancy because they felt I can’t gained enough. We barely even talked about weight in the second pregnancy, as neither one of us felt it was a great indicator of health. I’m really thankful for that. Personally, I struggled seeing the numbers go up both times because I felt like there was such scrutiny over my prenatal weight, bump size, etc. I don’t think there actually was, but our culture is so fit-obsessed. Even being a relatively fit mom, I felt large – which is really sad. Pregnancy is beautiful. We should all feel beautiful during this miraculous time.
I still wish this article came out and said, “for some women, gaining 40 pounds is fine.” No one says that.
I have always grown up with a number higher and heavier on the scale than people expect for how I look. I honestly don’t know if I have truly high bone density or what, but I have never weighed less than 135 pounds as an adult, even when I was 24 years old and a size 2 (I am 5’5″). When I was in the Army, the nurses would weigh me, do a double take, say “That can’t be right,” and then I would have to answer, “Yes, it’s right” and do a tape test to pass my physical fitness test.
Throughout my entire adult life, I have regularly had a 6″ wrist and a 27″ waist and 40″ hips with a really good hip to waist ratio, but weigh around 145 pounds, right on the edge of “overweight” with BMI.
It is so discouraging to me that if I put into a calculator that I am 5’5″ and weigh 148 pounds, the recommendation is that I can gain up to 35 pounds, but if I start at 150 (which I did with this pregnancy) suddenly I am only supposed to gain 25 pounds. I can say to myself, rationally and logically, just to ignore that 2-lb BMI difference and gain the 35 pounds, but it still makes me feel like such a failure to see that “above recommended weight gain of 25 lbs” constantly.
My body is very hourglass shaped. In the first three months of pregnancy, before I was even showing, I went from a 34″ chest to a 38″ bust line. At 32 weeks, it’s now at 39″. I wish there was more discussion of body SHAPE as well as size.
I have read your book, real food for gestational diabetes.
I’m currently 34 weeks and gained 27 pounds despite going on very low carb at 20 weeks and metformin. A few days ago I was prescribed insulin as metformin has not been helping. I’m worried about the weight gain. This is my first gestational diabetes pregnancy (3rd pregnancy) and my first time gaining so much weight. With my previous pregnancies I was not low carb, low GI and gained only 25 pounds total. Very confused as to what is happening and MFM just says it’s normal, you’re pregnant.
Great article!! I see you mentioned “newer research” supporting a higher weight gain for underweight parents. I can’t seem to find that studies specific to this recommendation. Do you happen to know which studies reported a weight gain above the standard recommendations is beneficial for pregnancy outcomes?
Thank you for this article. Not one of the easier topics to write about!
I have just a little item to point out: in the list of places weight is distributed during pregnancy, the placenta is listed twice. An easy oversight!
Thanks again 🙂
Very cool article. I’d love to see the “newer research” you mentioned too.
I’m currently 34 weeks pregnant with my fourth, no history of diabetes or gestational diabetes, no history of pre-eclampsia or high blood pressure, honestly I have healthy babies when all is said and done! I have nearly always been obese (39ish BMI before this pregnancy) and try to eat healthy and exercise as I am able.
My first pregnancy I gained 11 pounds, second I gained 23 pounds, and my third I gained around 9 pounds in the end. This pregnancy total – I’ve lost six pounds. I gained and lost all through the pregnancy and I was starting to worry at this last appointment. I was really happy when a friend pointed me to this article and I’d really love to see the research you referenced. Thanks!
This is very interesting to me. I am naturally “underweight”. Have been my whole life. And yet during pregnancy I only gained 9 kg. My baby was a healthy 3400 grams, plenty of fluid, no issues or complications. Yet it seems strange to me that I’d only gain so little if so so much more is considered healthier. I can’t imagine how much I’d have to overstuff myself in order to gain that much extra weight. I’m nauseated just thinking about it, but obviously want to make sure I do actually gain enough in future pregnancies.
Thank you for the article. I have bad experiences with discussing weight with doctors in general (but not during pregnacy since I havn’t been pregnat yet)
I would like to open a related topic – how to manage your weight when trying to concieve?
I really need to lose weight (I am currently at 209 pounds). “Eat healthy and move more but no strict diets” just doesn’t work (I’m already trying, maybe it would work if I would be really very strict about that, 0 mistakes, but being very strict about anything is not sutainable) but we don’t want to postpone the baby (trying already for 10 months). Is there any option? I have a feeling that I have to do something more radical to finaly start loosing weight but I don’t think it would be safe for the baby (who I’m not sure if is there every month 🙂 + I understand that right nutrition before conception is also important).
(I was obese as a child until my age 15-29 (with series of diets, struggling with maintainig healthy weight). Then I gained 50 pounds in 2 years, 33 pounds out of that in a few months (I am not sure what was the reason, probably a combination of calories restrincting – meaning low fat – diets before, stress eating including sweets, and hypoactive thyroid), in any case it wasn’t like overeating all the time and that fast weight gain didn’t feel natural (however, my endocrinologist made it pretty clear that it is mostly my fault). Most of that 2 year period I was actually trying to lose weight. Now we are trying to have a baby, so my friend told me about you, I have been trying to eat as you advise (but not perfectly with no mistakes) and walk more. It is finally a nutrition that makes sense to me but no weight loss occured (which is understandable since this is meant for pregnancy, not for weight loss + I’ve been cheating). But I don’t know what else to do.)