When it comes to pregnancy, arguably the most commonly discussed nutrient is folate. Almost all medical professionals will recommend a supplement of this nutrient prior to and during pregnancy because it’s known to help reduce the risk of neural tube defects (which can impact baby’s brain or spine).
Low folate status in a mother is also linked to a higher risk of congenital heart defects, having a low birth weight infant, and preterm birth.
Make no mistake—folate is a vital nutrient for a healthy pregnancy.
The form of supplementation that’s often recommended, however, is a synthetic version of the vitamin called folic acid. This is unfortunate, as this article will explain in detail.
What is folic acid?
Folic acid is a synthetic (meaning manmade) version of folate, otherwise known as vitamin B9. Folate is vital to many functions in your body and especially important before and during pregnancy for fetal development.
In order for your body to put folic acid to use, it must first be converted into the active form, known as 5-MTHF (short for 5-methyltetrahydrofolate).
Put another way:
“Folic acid itself is inactive in the human body, but is a precursor to the bioactive molecule 5-methyltetrahydrofolate (5-MTHF), which is formed in the liver by hepatic reductases.”
Most of the folate in your body is in the form of 5-MTHF. In fact, 5-MTHF represents 95–98% of folate in serum or red blood cells (RBCs).
This form of folate has been “methylated,” which means it can participate in a series of important processes in your body, as explained here:
“5-MTHF functions as a methyl donor in many metabolic reactions, including the conversion of homocysteine into methionine, the biosynthesis of glycine from serine, and the biosynthesis of DNA precursor molecules. Therefore, folate is fundamental for growth, especially in the embryonic and fetal stages.”
How is folic acid different from folate?
Folic acid is structurally and functionally different from folates that exist naturally in food. I say “folates” because there are many different forms of folate found naturally in food. For this reason, nutrition research refers to them as “food folates.” While over 150 different forms of naturally occurring folate have been identified, 5-MTHF is the major type of folate found in food. Folic acid is not present in whole foods (remember, it’s manmade); it is only present in foods that are fortified with folic acid.
The term folate is a catch-all for any type of folate, whether natural or synthetic. That means folic acid is a type of folate and 5-MTHF is another type of folate. For the purposes of this article, I will be specifying folic acid any time I’m referring to that form of folate.
Decades ago, folic acid was hailed as a necessary supplement to reduce the risk of neural tube defects and many practitioners recommend high doses of it, however not all people process folic acid well, particularly those who have a genetic variation in an enzyme involved in the metabolism of folate known as MTHFR.
Psst – The folate versus folic acid and MTHFR discussion has come up so many times that I’ve devoted several “research briefs” to the topic on my Instagram page. If you don’t yet follow me there, that’s the social media platform I post on most regularly (I’m @lilynicholsRDN). My research brief posts highlight specific studies related to preconception/pregnancy/postpartum nutrition and why they are relevant to you.
What is MTHFR?
MTHFR is short for methylene tetrahydrofolate reductase, an enzyme that’s involved in folate metabolism, methylation, and processing amino acids.
To quote the National Institutes of Health:
“Methylenetetrahydrofolate reductase is important for a chemical reaction involving the vitamin folate (also called vitamin B9). Specifically, this enzyme converts a form of folate called 5,10-methylenetetrahydrofolate to a different form of folate called 5-methyltetrahydrofolate. This is the primary form of folate found in blood, and is necessary for the multistep process that converts the amino acid homocysteine to another amino acid, methionine. The body uses methionine to make proteins and other important compounds.”
MTHFR can also refer to the gene that determines the function of the MTHFR enzyme. Typically MTHFR variations mean that there is a reduced ability to process folate, particularly folic acid.
When people say “I have MTHFR” what they’re really trying to say is that they have a MTHFR variation. In reality, we all have MTHFR, it’s just that some people’s MTHFR functions better than others. Make sense?
I use the phrase “genetic differences” or “genetic variations” because they are incredibly common, but you might also see them called mutations or polymorphisms or single nucleotide polymorphisms—SNPs for short. A genetic mutation sounds rather scary; genetic differences reminds us that these are not uncommon.
Why do MTHFR variations matter?
Estimates are that 40-60% of the population has at least one MTHFR polymorphism, which means that roughly HALF the population has an impaired ability to use synthetic folic acid.
This creates a major problem if we’re relying on fortified foods or supplements that have high levels of folic acid, particularly if the rest of our diet is low in food folate.
Thanks in large part to the work of Dr. Ben Lynch, more people are aware of this issue and are actively steering away from the cheap folic acid that dominates the multivitamin/prenatal vitamin world (not to mention what is fortified into refined grain products in the U.S. & other countries).
Instead, they are using more metabolically active forms of folate, such as methylfolate and folinic acid (note the extra “in” in folinic) when supplementing. More people are also emphasizing real food folate.
To be clear: Those of us with MTHFR variations (yes, I’m included in this group!) need metabolically active versions of folate. Our bodies have trouble processing synthetic folic acid.
Best types of folate if you have MTHFR
Technically, with or without MTHFR variations, we all benefit from using metabolically active forms of folate versus synthetic folic acid. So whether you’re an MTHFR carrier or not, this still applies to you!
Types of folate your body can process:
- Folates in food (highest sources include liver, legumes, leafy greens, and more; see the bottom of this article for a full list of folate-rich foods)
- Methylfolate* aka 5-MTHF (this is the dominant type of folate found in food; it’s also available as a supplement)
- Folinic acid** (this is NOT folic acid—note the extra “in” in folinic; this is sometimes found in supplements alongside methylfolate.)
Type of folate your body can’t process (or can’t process well):
- Folic acid
*Note that methylfolate can go by several different names on supplement labels. The best forms are L-methylfolate or L-5-methyltetrahydrofolate (also called 6(S)-L-methyltetrahydrofolate). If you want a crash course on this, see this post from Dr. Lynch. Heads up that it gets into some organic chemistry.
**Folinic acid is one step “behind” methylfolate in the folate cycle (bypasses DHFR). It is converted in the body into 5-MTHF. It’s beyond the scope of this article to get into the specifics on folinic acid, but for some people who do not tolerate supplemental methylfolate or for people undergoing specific medical treatments that interfere with folate metabolism, folinic acid is sometimes used.
But my doctor says only synthetic folic acid is proven to prevent neural tube defects?
This rebuttal comes up often and unfortunately, reflects a lack of understanding of nutritional biochemistry.
I’ll leave it to the folate researchers to explain how we’ve ended up in a quandary where we don’t have “enough” data to recommend the biologically active form of folate that is not only the primary type of folate in food, but also the primary form of folate in our blood, our red blood cells, and cord blood.
“Although there are no clinical trials on the effectiveness of 5-methylTHF in preventing NTDs [neural tube defects], metabolic studies have shown that 5-methylTHF is a biologically active form of the vitamin and it seems to be at least as effective as folic acid in improving folate biomarkers. The literature clearly shows that a better food folate intake is associated with better folate markers and that food folate can prevent NTDs (by increasing folate status). Folic acid can prevent NTDs by increasing serum or blood folate level. 5-MethyTHF can effectively increase serum or blood folate markers. Therefore, supplementing with 5-methylTHF for NTD prevention seems to be rational… [T]esting the efficacy of 5-methylTHF against a placebo would be unethical. Comparing the preventive effect of folic acid with a proposed better alternative (5-methylTHF) will require following several thousands of pregnancies over a long time. The costs of testing 5-methylTHF against folic acid would be extremely high. We do not have any reason to assume that a randomized controlled trial is justified before recommending 5-methylTHF.”
Here’s another researcher’s take:
“Folic acid itself is inactive in the human body, but is a precursor to the bioactive molecule 5-methyltetrahydrofolate (5-MTHF), which is formed in the liver by hepatic reductases. Folic acid is more heat stable than the active vitamin and costs much less, and is therefore the generally preferred form for production, sales and therapeutic use. However, this molecule is oxidized. It is naturally present in food in only trace amounts (Table 1) and molecular forms similar to folic acid are not found in nature. For these reasons, there has been much debate about the risk of side effects of folic acid supplementation and about the possible advantages of using its active form, 5-MTHF, which represents about 98% of all folate in plasma.“
The advantages of using methylfolate supplementation over folic acid include:
- Highly bioavailable; it is already a biologically active form with no need for conversion/activation
- It is the main type of folate in our blood (serum and red blood cells) as well as cord blood (fetal blood supply)
- It does not mask vitamin B12 deficiency, unlike folic acid (more on this topic below)
- It does not cause unmetabolized folic acid in the body (more on this topic below)
- Women with MTHFR polymorphisms show a better response with plasma folate markers to methylfolate
- It is effective at preventing neural tube defects
- There is no tolerable upper limit (i.e. low risk for toxicity, unlike folic acid)
Given all of the above, it’s no surprise that a 2020 review on folic acid vs. methylfolate in pregnancy concluded:
“Supplementation with 5-MTHF in pregnancy could be advantageous over that with folic acid, because 5-MTHF is immediately active, does not require metabolic activation, and is directly bioavailable to the mother and fetus and is not influenced by the possible MTHFR gene mutations.”
How do you know if you have MTHFR variations?
In short, to test for MTHFR, you’ll need a genetic test. Some health practitioners can order MTHFR testing for you, so ask first.
If that’s not an option, you can do an at-home testing for MTHRF, which typically uses a saliva sample or cheek swab that you mail in to the company for analysis. This is my favorite one on the market developed by a doctor who specializes in genetic variations and their effect on health (no, this company did not sponsor this post, but I do earn a small affiliate commission if you choose to purchase it). The report is also far more comprehensive than any others I’ve seen.
If you don’t have the opportunity/finances to get genetic testing, there is no harm in prioritizing real food folate and checking that your supplements provide metabolically active forms of folate (in other words, you can simply play it safe by avoiding folic acid).
Why is folic acid used in supplements/food fortification if better alternatives exist?
It’s a good question and the answer is simple: money.
Methylfolate is more expensive than folic acid—and by quite a bit!
According to Dr. Ben Lynch of Seeking Health supplements, this is the cost breakdown for sourcing the raw materials (as of 2020):
- Folic acid costs roughly $50 per kilo
- Folinic acid as calcium folinate costs $1,800 per kilo
- 5-MTHF as Quatrefolic costs $13,300 per kilo
That means a supplement company will pay upwards of 266x more for using methylfolate in their product. They have to CARE to make that choice, not just be focused on maximising profits. I’ve been shocked to see that even many “pharmaceutical grade” prenatal vitamins often contain cheap synthetic folic acid. It’s like they’re stuck in the 90’s or just don’t care.
Aside from the higher cost, it’s taken a few decades for enough research to accumulate on the potential downsides of folic acid for people to question if we could do better. See my answer to the above question “But my doctor/perinatologist says only synthetic folic acid is proven to prevent neural tube defects?” for more on this.
Remember, folic acid doesn’t occur in nature—it’s manmade. Originally, researchers thought folic acid was superior to food folates because it is stable and very efficiently absorbed from the GI tract. That’s true, however absorption efficiency doesn’t matter if it’s not well utilized in the body. Absorption and utilization are two separate things.
The problem with supplemental folic acid & unmetabolized folic acid
Speaking of poor utilization… There’s now abundant research showing that excessive folic acid can build up in the body. Researchers call it “unmetabolized folic acid” or UMFA.
“Dietary supplementation coupled with pervasive fortification of grain-derived foods with synthetic folic acid beginning in the late 1990s may have created a demographic with high serum levels of unmetabolized folic acid and high erythrocyte folic acid concentration. This is not theoretical, but has been demonstrated in a dose-dependent manner when levels of intake are over 200 mcg per day. Folic acid is detectable in fasting serum of a majority of subjects tested, and the proportions with detectable levels have risen since fortification programs were initiated.”
It’s counter intuitive, but high levels of folic acid can interfere with the very metabolic processes that folate supports, particularly methylation.
You’d think this is only a concern for those with MTHFR variations, but that’s not true.
It’s certainly more important for them, but it doesn’t mean everyone else is in the clear to consume large amounts of folic acid without side effects. Keep reading for more on this.
Unmetabolized folic acid has also been shown to accumulate in fetal blood supply in mothers who are supplemented with folic acid. (For some shocking stats on UMFA in pregnancy and in babies, see this section below: “What about the safety of folic acid during pregnancy?”)
This is why researchers who actually comprehend the biochemistry keep returning to essentially the same conclusion:
“In light of our understanding of folate metabolism, there is growing concern about the risk to the fetus of high levels of inactive metabolites of folic acid, for both their oxidizing effects and a possible association with vitamin B12 deficiency. Instead, the administration of equimolar doses of 5-MTHF enables reaching the same target of maternal serum folate without generating inactive metabolites.”
But isn’t folate deficiency rampant?
There’s no question that prioritizing folate intake is important to fertility and pregnancy. However, actual deficiency in folate is less common than you’ve been led to believe.
According to a 2017 analysis of NHANES data (which is a nationally representative dietary survey in the U.S. from a diverse socioeconomic background), the average intake of folate among women ages 19-50 was on par with the recommended dietary allowance for pregnancy of 600 mcg (range 635 – 702 mcg/day).
Only 11% of women consumed less than the estimated average requirement, which is 320 mcg. Almost none of the women had low serum folate levels, but a shocking 37-39% had elevated serum folate.
Unfortunately, this study did not look at levels of unmetabolized folic acid (UMFA) specifically, but given that a folic acid intake as low as 200 mcg can result in elevations in UMFA, it’s likely that much of the folate in those with elevated serum folate levels was in the form of UMFA. This could pose a problem to fertility and pregnancy, as I’ll discuss below.
Now also consider that the majority of pregnant women in the U.S. (77% according to NHANES) take a prenatal supplement that contains folic acid with an average dosage of 817 mcg folic acid. In addition, those who take a prenatal vitamin or supplemental folic acid are the most likely to consume adequate folate from their diet (including foods fortified with folic acid). That means many women may be exceeding the tolerable upper limit of folic acid when you assess dietary and supplemental folic acid together.
How much folate do you need in pregnancy?
Recommended Dietary Allowance: 600 mcg for pregnancy; 400 mcg non pregnant female
Tolerable Upper Limit: 1,000 mcg
Note that there is no tolerable upper limit for food folates. The tolerable upper limit applies specifically to folic acid.
Do people with MTHFR need more folate?
First off, those without MTHFR variations are recommended to take in 400-600 mcg of folate in the 2-6 months leading up to pregnancy with the goal of normalizing serum folate levels prior to conception. During pregnancy, continue to aim for a minimum of 600 mcg per day.
Research suggests that those with MTHFR variations often have lower folate status and therefore may need a dosage of 800 mcg per day to normalize serum folate levels prior to conception and to maintain adequate folate levels during pregnancy. Also note that MTHFR carriers have higher choline needs and choline is equally important for reducing the risk of neural tube defects (more on choline in this comprehensive article).
What about taking synthetic folic acid prior to conception? What about taking folic acid if I don’t have MTHFR variations? Is methylfolate still better for fertility?
Many practitioners are not familiar with the biochemistry of folate and continue to push folic acid supplements on fertility/pregnant clients, often in really high amounts (sometimes 5x the established upper limit for folic acid). This would present a clear problem for someone with an MTHFR variation, but even without it, it’s still wise to avoid high doses of synthetic folic acid.
In one case study, a woman with a history of infertility with no mutations in her MTHFR gene had been instructed to take 5,000 mcg of folic acid prior to an assisted reproductive treatment. This is a very common recommendation in reproductive endocrinology. Again, note that the upper limit for folic acid is 1,000 mcg/day.
After 4 months of treatment, her homocysteine (a marker of inflammation) had jumped 40%. Folic acid was discontinued and in its place, 500 mcg of methylfolate was used. Note that the dosage of methylfolate was 10x lower than the dosage of folic acid she was previously given.
Within 5 days on methylfolate, her homocysteine dropped to the normal range. Just as the research has shown in animal models, synthetic folic acid is not only inefficiently metabolized, but it can actually have the opposite effect of what’s intended.
The authors explain:
“It is now clear that the practice of prescribing high doses of synthetic folic acid should be at least a matter for debate. 5-MTHF, the “active” folate that is immediately available for conversion of homocysteine to methionine, should be proposed instead of folic acid for periconceptional support and even for nutritional supplementation in general.”
This makes sense when you understand the biochemistry. As one study explains:
“Folates often show strong substrate inhibition of the enzymes that make use of them, and modeling studies suggest that high folate levels could, under certain circumstances, have the same functional effect as low folate status.”
I’m going to repeat that past part: “…studies suggest that high folate levels could, under certain circumstances, have the same functional effect as low folate status.” That means you could be causing a functional folate deficiency by taking high dose folic acid.
It’s also concerning that elevated homocysteine is an independent risk factor for miscarriage. The link between this inflammatory marker and miscarriage has been known for decades. High homocysteine is also linked to injury in the vascular structures of the placenta that form early in pregnancy, potentially resulting in “various obstetric complications such as recurrent pregnancy loss, fetal growth restriction, preeclampsia, abruption placenta, and stillbirth.”
If high dose folic acid is actually causing increased inflammation as evidenced by elevated homocysteine, it seems logical to me that this is NOT an appropriate intervention to “improve fertility.”
Case in point… In another study, 16 women with recurrent miscarriage (that’s 3 or more in a row prior to 20 weeks gestation) who also have a MTHFR variation were given a combo of methylfolate, vitamin B6, and vitamin B12.
After 6 months, this combination of nutrients was shown to reduce levels of homocysteine from an average of 19.4 ± 5.3 μmol/L to 6.9 ± 2.2 μmol/L. That’s an almost 3-fold drop, bringing average homocysteine levels from a harmful range to the normal range.
It also helped 7 of the 16 participants conceive and carry to term within 1 year.
I especially like this study for three reasons:
- It uses the proper form of folate versus folic acid (surprisingly rare in research studies on fertility)
- It uses a synergistic combo of B vitamins instead of trying to “fix” everything with folate alone
- It illustrates the power of nutrition for a very common and heartbreaking problem
Now, one final consideration for folate vs. folic acid in regards to fertility is the partner. As the saying goes, it takes two to tango and when it comes to folic acid, concerning findings have been found in relation to sperm health in men supplemented with synthetic folic acid. These observations have been documented in both human and animal studies. Men with MTHFR variations are even more at risk for sperm abnormalities when they consume excessive quantities of synthetic folic acid.
UPDATE: I cover much more research on the impact of forms of folate and MTHFR variations in relation to female and male fertility in this 2-hour webinar on folate for healthcare professionals.
What about the safety of folic acid during pregnancy?
When it comes to pregnancy, research has shown that prescribing high doses of folic acid to pregnant women results in maternal and cord blood levels of unmetabolized folic acid 5x greater than normal. Many studies have also documented high levels of unmetabolized folic acid in newborn infants, even in areas without mandatory food fortification programs.
Unmetabolized folic acid is a bigger problem in countries who fortify their food supply with folic acid (~80 countries worldwide have fortification programs). In one Canadian study, 93% of newborns had detectable unmetabolized folic acid present in their blood (notably, 90% of mothers in this study were taking supplemental folic acid, most commonly in a dosage of 1,000 mcg per day).
The high dosage of folic acid supplementation often given in pregnancy is worrisome because it doesn’t take much to negatively affect folate metabolism in the body.
Consider this from a 2015 study:
“Folic acid intake as little as 280 mcg saturates the capacity of dihydrofolate reductase, which is a critical step in folic acid metabolism and results in its appearance unaltered in the circulation.”
The phrase “unaltered in the circulation” is another way of saying that some of this folic acid does not get utilized by the body, meaning you have unmetabolized folic acid present in your blood.
If you think what I’m sharing here is shocking, consider this from a 2015 research paper in the esteemed American Journal of Clinical Nutrition looking at unmetabolized folic acid in cord blood:
“…[B]ecause of concerns over potential adverse health outcomes, the functional ramifications of the observed high concentrations of folate and UMFA in maternal and fetal circulation in the current study warrant additional investigation. Specifically, the dose of folic acid in prenatal supplements should be reconsidered in light of our findings to provide the optimal health benefits to the growing fetus while avoiding undue risk.”
The take home message here is that we don’t fully understand the side effects of unmetabolized folic acid. If we don’t understand something fully and it could pose possible side effects, it should at least give us pause. High levels of UMFA as a result of folic acid supplementation has been linked to a higher risk of neonatal jaundice, infant asthma, developmental delay, and even autism.
I know the last word in that sentence is especially worrisome for parents-to-be. With regards to the suspected link of high folic acid intake and autism, here’s what a 2017 study has to say:
“[A]lthough optimal levels are important for development, there is no known benefit to exceeding the RDA for folates, and yet this is occurring. It is clear that some women are taking more than 1000 mcg a day while they are pregnant. There is experimental animal and in vitro research documenting negative effects of excess or unmetabolized FA on genetic programming and neuronal development. At least three studies have suggested that high levels of supplementation when taken throughout pregnancy may be associated with negative neurodevelopmental outcomes in offspring. As a whole, caution regarding over supplementing is warranted.”
Keep in mind, however, that not all studies are in agreement on the possible link between folic acid and autism. Remember that adequate FOLATE is key for normal brain development. It’s likely that problems with methylation as a whole impact autism risk and that high dose synthetic folic acid taken outside of the context of a diet that contains ample nutrients that support methylation more accurately reflects the potential increased risk of neurodevelopmental issues related to folic acid.
For example, a study from Spain found that high dose folic acid supplementation of 5,000 mcg per day was linked to delayed psychomotor development. Furthermore, a 2017 study found that 4-5 year old children of mothers who supplemented with greater than 1,000 mcg of folic acid before and during pregnancy scored lower on global verbal, verbal memory, and several others measures of cognitive function, an effect that was not seen in mothers who consumed folic acid in doses below 1,000 mcg per day. The authors concluded: “Pending confirmation from further studies, the use of folic acid supplement dosages of 1000mg/d during pregnancy should be monitored and prevented as much as possible, unless medically prescribed.”
It would be far more prudent to encourage the consumption of whole foods that provide an array of nutrients that support methylation, rather than providing synthetic folic acid in high doses, but I digress.
Nutrition research so often compartmentalizes findings and tries to identify the “magic bullet” when no such thing exists. Your body needs folate in combination with ample choline, vitamin B12, vitamin B6, riboflavin, glycine, magnesium, trace minerals, and betaine (among other nutrients) to properly support methylation and folate metabolism.
UPDATE: For health professionals who want a deeper understanding of folate metabolic pathways, research on risks of autism, and more, please see this 2-hour Women’s Health Nutrition Academy webinar on Folate & Methylation in Fertility & Pregnancy.
Is there a link between synthetic folic acid and tongue ties?
When I polled my social media for their questions and concerns about folate, one of the most common was whether or not there’s a link between tongue ties (also called ankyloglossia) and synthetic folic acid.
There are conflicting opinions on this topic and by no means is the research settled. Population-wide, it seems as though rates of tongue ties are increasing, however some argue that this is a matter of increased awareness or a result of a higher breastfeeding rate, thus more ties are being identified that would have otherwise not been in previous years. Obviously, mothers of tongue tied babies would disagree. Anecdotally, many of the midwives I’ve talked to who have been practicing for decades feel that it is indeed a growing phenomenon in recent decades.
Studies seem to support that observation as data from the U.S., Canada, and Australia report increasing rates of tongue ties as well as corrective procedures for tongue ties. For example, in Australia, from the years 2006 to 2012, rates of frenotomy (which is the name of the procedure to release a tongue tie) went from 1.22 per 1000 children in 2006 to 6.35 per 1000 in 2016.” That’s an increase of 520%.
As far as rates of frenotomy in Canada and the U.S., “Increases have similarly been reported for British Columbia in Canada (2004–2013: 89% increase) and the United States (1997–2012: 866% increase).”
Some have questioned whether this is related to fortification of the food supply with folic acid, which began (in the U.S.) in 1998 or with the public health campaign to take folic acid supplements preconception, potentially resulting in over exposure to synthetic folic acid.
The theory is that because folic acid is involved in the formation of organs and mid-line structures, that it’s possible for higher folic acid supply during organogenesis (which takes place in the first trimester of pregnancy) might result in “tighter closure of mid-line structures.” In other words, the concern is that excessive folic acid could result in thicker tissues in the mid-line, such as the frenulum under the tongue (tongue tie) or that connects the lip to the gum line (lip tie).
A 2020 observational case control study looked at 85 infants with tongue ties compared to a control group of 140 infants without tongue ties and whether there was an association with folic acid intake of their mothers.
When the researchers looked at folic acid intake at “any intake” level, there was only a “slight, insignificant elevated frequency” of tongue tie. But, when they analyzed those who reported intake of preconception folic acid “on a regular basis,” the incidence of tongue ties was significantly higher among babies exposed to folic acid (54.1% vs. 25.7%), representing a 2-fold higher risk. They decided to analyze preconception intakes separately because the frenulum is formed by approximately week 6 of pregnancy, therefore preconception intake (as opposed to mid-to-late pregnancy) is a more accurate reflection of folic acid exposure during the time when a tongue tie develops.
What I found interesting was that folic acid intake was not reported to be very high in this study. The average dose of folic acid was 400 mcg per day and only four women took folic acid doses in excess of 1,000 mcg per day.
The study goes on to explain that the “association between regular folic acid intake and ankyloglossia in our study was not related to supra-physiological doses.”
Some would argue that this study’s findings are not accurate because the mothers were asked about folic acid intake after the birth of their child (a risk for recall bias), however the authors explain that “mothers in both groups were not aware of the study hypothesis, thus such bias is not likely to explain the difference.“
Now, this is the first study of its kind, so we’ll need to see more data before we draw strong conclusions here.
It would be nice to have a study looking at levels of unmetabolized folic acid in early pregnancy and whether that’s linked to tongue ties, however such a study would be really hard to pull off as most women do not know they are pregnant until after the structures of the tongue have already formed.
Nonetheless, this study further reinforces that synthetic folic acid is not without risks. There is so much we simply don’t know yet.
Folic acid and vitamin B12 deficiency
One of the well-documented risks with excessive folic acid supplementation is that it can mask a type of anemia called megaloblastic anemia. Megaloblastic anemia can be caused by either a deficiency in folate or vitamin B12 (or both) because both nutrients are involved in red blood cell (RBC) synthesis.
Lack of either vitamin leads to the production of abnormally large RBCs with a decreased ability to carry oxygen. Because the metabolism of folate is dependent on B12, deficiency of either one of these nutrients manifests as megaloblastic anemia, and furthermore, it takes a skilled clinician and several lab tests to differentiate between which nutrient is the cause.
In the case of pregnancy, excessive intake of folic acid is more common than excessive vitamin B12 intake, sometimes resulting in the appearance of “normal” red blood cells via lab testing, but with a “hidden” vitamin B12 deficiency present. These cases are more likely to present with neurological or systemic symptoms of vitamin B12 deficiency, such as poor memory, muscle cramps, or nerve tingling versus typical anemia symptoms.
People who follow vegetarian diets should take note and be sure they are supplementing adequately with vitamin B12.
Some researchers caution that folic acid not be supplemented without simultaneously providing vitamin B12. One paper goes so far as to say “one should never prescribe folate supplementation alone without the concomitant prescription of vitamin B12.”
But again, the issues caused by folic acid supplementation are a non-issue when supplementing with 5-MTHF, as explained here (bold emphasis added by me):
“[B]ecause folic acid triggers the synthesis of tetrahydrofolate without the need for vitamin B12, supplementation with this vitamin could resolve anemia due to vitamin B12 deficiency and not to a real deficiency of folate. This effect cannot happen when 5-MTHF is administered. Therefore 5-MTHF presents a lower probability of concealing hematological symptoms due to vitamin B12 deficiency.”
In simple terms, you don’t need to worry about the vitamin B12 issue if you are receiving folate from food or in the 5-MTHF version via supplements.
UPDATE: Since releasing this post, practitioners have asked for more in-depth information on folate. Our 2-hour professional level webinar covers the issue of vitamin B12 deficiency and the so-called “methyl trap” more extensively. Check it out here.
How can you avoid exposure to excessive amounts of synthetic folic acid while still receiving enough folate?
Hopefully you’ve actually read through this giant article and understand the importance of FOLATE, but the downsides of synthetic FOLIC ACID.
There are two places you’re getting folic acid:
- Supplements
- Fortified food
Common places where folic acid is found include a multivitamin or prenatal vitamin, B vitamin complexes, folic acid supplements, fortified nutritional yeast, energy drinks, enriched white flour and grains, and some nutritional drinks/shakes/bars with added folic acid.
Finding a supplement or prenatal WITHOUT folic acid
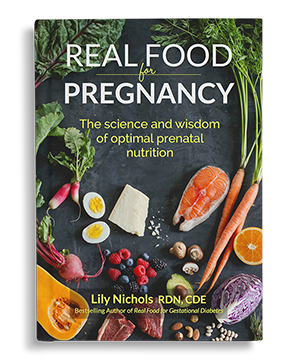
I believe the majority of pregnant clients benefit from a prenatal vitamin, you just have to be really picky about the quality, so you get the appropriate form(s) of folate. There are many, many other considerations when choosing a prenatal, which are detailed in Ch 6 of Real Food for Pregnancy. For the sake of simplicity, here are two comprehensive prenatal vitamin formulations I recommend: Prenatal 1, Prenatal 2.* For additional options, please follow the link in Ch 6 of Real Food for Pregnancy to get a free downloadable guide with additional prenatal vitamin/supplement options.
*Full disclosure: these are affiliate links, meaning I receive a small % commission on your purchase, but the product does not cost extra to you. This small commission does not influence my decision to back these brands. Believe me, companies ask me constantly to promote their products and I turn down 99.99999% of them.
Identifying food sources of synthetic folic acid
As for FOOD sources of synthetic folic acid, you’re looking at products that have ADDED folic acid. These are called “fortified” or “enriched” foods and primarily comprise products made with white flour or other refined grains.
I’ll be addressing this from an American perspective, as we have a mandatory fortification program for refined grains that are sold across state lines. If you live in a different country, you may or may not have a fortification program (~80 countries DO have a mandatory fortification program). If you do, the levels of folic acid may be at different concentrations than the U.S.
According to the USDA, most “enriched” breads, flours, corn meals, rice, noodles, macaroni, and other grain products must include 140 mcg of folic acid per 100 grams of flour.
How much folic acid are you getting from fortified foods?
In real world terms, a typical slice of white bread (which, in the U.S. is made with enriched flour that’s fortified with folic acid) provides 25-50 mcg of folic acid. One cup of cooked spaghetti contains 102 mcg. One cup of cooked enriched white rice provides 115 mcg. One packet of instant oatmeal provides 80 mcg. Nabisco’s Ritz crackers provide 46 mcg per 20 crackers.
Some breakfast cereals provide far greater amounts. For example, Raisin Bran provides 150 mcg of folic acid per cup while the General Mills cereal TOTAL provides 400 mcg of folic acid in a ¾ cup serving. Multigrain Cheerios provide 408 mcg folic acid per serving (alongside a mere 6 mcg of food folate; so much for “whole grains” being nutrient-dense, eh?).
Since most people do NOT measure their portions of cereal, many are consuming above and beyond the RDA of folate in the form of synthetic folic acid from their breakfast alone.
If you’re eating fortified grain products, which most Americans are, that means that many women are already consuming excessive quantities of folic acid before you even factor in prenatal supplements. Then, consider that 85% of the carbohydrates consumed in the U.S. diet are from refined carbohydrates and you can see we can run into problems here.
Earlier, I pointed out studies showing an intake of folic acid of 200-280 mcg can disturb folate metabolism in the body. It would be very easy to overdo it if your diet includes breakfast cereal or any products made from white flour on a regular basis. That appears to be the case, as American women take in an average of ~300 mcg of synthetic folic acid on a daily basis. The FDA’s estimate was that fortified food would add only 140 mcg to an adult’s intake, but that obviously is not the case for most Americans.
Overall, I recommend limiting synthetic folic acid to no more than 200 mcg/day. Intake below this level does not appear to drastically disturb folate metabolism in the body. If you want to avoid folic acid entirely and get your folate from real food sources or better supplemental forms, no problem, but that’s tricky if your diet contains any amount of refined, fortified carbohydrates.
Real food matters for more than just folate
I’ve long been an advocate of a real food diet for pregnancy, which is one that is made primarily of foods that have not been processed in a way that reduces their nutritional value. Refined grains, by default, are processed to remove nutrients and then food scientists attempt to replace part of what was lost with synthetic vitamins. In situations of extreme food scarcity, this is better than unfortified white flour, but it’s not ideal.
In addition to the issues with synthetic folic acid, refined grains are high-glycemic, meaning they spike blood sugar. Elevated blood sugar has a slew of its own problems related to fertility and pregnancy, including increasing the risk of birth defects (yes, neural tube defects included).
Wouldn’t it be better to get your folate from REAL FOOD and in a form (or forms) that your body recognizes and can appropriately metabolize? That’s what I believe should be emphasized for optimal fertility and pregnancy outcomes.
Real food sources of folate
Here are a few examples of foods that are naturally rich in folate—the REAL thing. All quantities are based on a 100g serving. That means the folate content is listed by weight of the food, but I included a real world serving size equivalent as well so you don’t need a food scale to estimate your intake.
Pro tip: If you’re searching nutrient databases for folate rich foods, you must be sure to search for “food folate” otherwise, you’ll get a bunch of fortified foods showing up as your “best” sources. Don’t be fooled. Those products contain synthetic folic acid. I specifically did not include any fortified foods in the list below.
The term folate comes from the word foliage, meaning green leaves, hence many of the sources of folate are from plants; however, it may surprise you that some animal foods are actually far more concentrated in folate than plants. After all, animals eat plants (or eat animals that eat plants) and thus become a concentrated source of said nutrients.
Animal foods — 100g is approximately a 3.5 oz serving
Liver (duck) 738 mcg
Liver (turkey) 691 mcg
Liver (chicken) 588 mcg
Liver (lamb) 400 mcg
Giblets (chicken) 367 mcg
Egg yolk 146 mcg, about 6 yolks
Kidney (beef) 98 mcg
Fish roe 93 mcg
Legumes (beans/lentils), Nuts, Seeds — 100g
Sunflower seeds (roasted) 238 mcg, about ⅔ cup
Lentils (cooked) 181 mcg, about ½ cup
Chickpeas/garbanzo beans (cooked) 172 mcg, about ⅔ cup
Black beans (cooked) 149 mcg, about 1.25 cups cooked
Peanuts (roasted) 145 mcg, about ⅔ cup
Kidney beans (cooked) 130 mcg, about ⅔ cup
Sesame seed butter (tahini) 115 mcg, about 7 Tbsp
Hazelnuts 113 mcg, about ⅔ cup
Split peas (cooked) 65 mcg, about ½ cup
Vegetables & plant foods — 100g
Wakame (seaweed, raw) 196 mcg, 1.25 cups
Spinach (raw) 194 mcg, about 3 cups
Asparagus 191 mcg, about 3 oz
Kelp 180 mcg, about 1 cup
Parsley (raw) 152 mcg, about 1.5 cups
Romaine lettuce 136 mcg, about 2 cups, shredded
Turnip greens (cooked) 118 mcg, about ⅔ cup
Beets (raw) 109 mcg, about ⅔ cup
Broccoli (raw) 109 mcg, about 1 ⅓ cup
Brussels sprouts (raw) 109 mcg, about ¾ cup
Collard greens (cooked) 98 mcg, about ½ cup
Arugula (raw) 97 mcg, about 5 cups
Avocado 89 mcg, about ⅔ of a medium Hass avocado
Artichoke hearts 87 mcg, about ⅔ cup
Interestingly, as I looked at the nutrient databases on folate content of foods, not all green leafy vegetables were good sources of folate. Some examples that surprised me were beet greens (raw), which provided only 15 mcg per 3 cup serving (100g) and kale (raw) which provided 29 mcg per 2 cups serving (100g). As always, nutrient databases are not perfect, since nutrient levels can vary in foods depending on how they’re grown, how quickly they were processed after harvesting, variety of the plant, and more factors. Still, I found it interesting to see that organ meats and legumes could provide ample folate in folks who do not enjoy or eat much in the way of leafy greens.
Keep in mind that different preparation methods can reduce folate concentrations. Pre-chopping vegetables, for example, can result in a loss of folate due to oxidation. In addition, soaking, boiling, steaming, freezing, thawing, roasting, frying, microwave heating, homogenization, preservation of canned food can all reduce folate levels. I was surprised to find out that freezing vegetables can result in a 12-22% loss of folate. As always, the least amount of processing, the better. In the above list, I listed the folate content for the food as either raw or cooked based on the way that food is most commonly consumed. You might like to read this post on raw vs. cooked vegetables for more on this topic. Don’t worry. You don’t need to become a raw foodist!
What does a diet rich in food folate look like?
When I created the meal plans in Real Food for Pregnancy, providing ample folate was one of the top considerations. The nice thing about a real food diet is that it’s not very hard to meet folate needs from food. All of my meal plans exceed the recommended dietary allowance for pregnancy of 600 mcg per day; they even outperform the conventional prenatal meal plans that rely on fortified foods. You can see a sample meal plan alongside a nutritional breakdown in the first chapter, which I give away free here on my site (see bottom of this post or the freebies page).
A few examples of food folate-rich meals and snacks:
- Snap peas or broccoli with hummus (hummus contains both chickpeas and tahini)
- Eggs and sauteed spinach
- Spinach quiche (recipe in Real Food for Pregnancy)
- Spinach dip (recipe in Real Food for Pregnancy)
- Liver pate
- Hidden liver in any ground meat dish (see recipe for meatloaf in Real Food for Pregnancy, meatballs, Shepherd’s pie, and Indian Spiced Stuffed Bell Peppers)
- Shaved Brussels sprouts salad
- Avocado (added to basically any meal/snack—guacamole anyone?)
- Avocado stuffed with fish roe
- Apple + peanut butter
- Arugula salad with artichoke hearts, shredded beets, and sunflower seeds
- Tabouleh (Mediterranean salad made with lots of fresh parsley)
- Romaine salad with avocado, chickpeas, and hard boiled egg
- Beets (prepared any way you like—pickled, beet slaw, roasted, etc.)
- Lentil soup
- Sunflower seeds, peanuts, or hazelnuts as a snack
- Roasted Brussels sprouts
- Split pea soup
I could go on and on…
Summary: folate is important, but the form of folate you take matters, regardless of your genetics.
Alright, we’re over 7,500 words in now. Have I lost you yet?
The take home messages about folate and why it’s superior to folic acid for pregnancy and fertility (and all life stages, let’s be real) are as follows:
- Folate is an umbrella term that includes food-sourced and metabolically active forms of folate (like methylfolate), and is also used to describe the poorly metabolized, synthetic version known as folic acid.
- Most of the folate in your body and most of the folate found naturally in foods is in the form of methylfolate (specifically 5-methylfolate or 5-MTHF).
- Those with MTHFR variations (40-60% of the population) have a reduced ability to metabolize folic acid and convert it into methylfolate; these people need to be especially careful to avoid synthetic folic acid and opt for metabolically active forms of folate instead.
- Moderate and high intake of folic acid can disturb folate metabolism (and methylation) in the body (even in people without MTHFR variations), potentially contributing to inflammation, infertility, and adverse pregnancy outcomes; The OPPOSITE is true of natural forms of folate.
- A diet rich in food folate alongside a high quality prenatal vitamin that contains metabolically active forms of folate is optimal. In pregnancy, aim for 600-800 mcg/day.
- Using food-sourced folate or folate in metabolically active forms avoids any risk of “unmetabolized folic acid” in your system or any of the documented risks of folic acid supplementation.
- If you consume fortified foods, aim to keep synthetic folic acid intake to less than 200 mcg/day to avoid disturbing folate metabolism in your body. In short, there are risks with high intake of folic acid whereas there is no risk with food sourced or metabolically active folate.
- Multiple nutrients are involved in the metabolism of folate. Think beyond single nutrients! Your body needs folate in combination with ample choline, vitamin B12, vitamin B6, riboflavin, glycine, magnesium, trace minerals, and betaine (among other nutrients) to properly support methylation and folate metabolism.
Know the difference between the different types of folate and why folate is superior to folic acid in pregnancy and in all stages of life. It matters! Make sure your healthcare provider knows the difference as well.
Feel free to share this article to spread the word!
Let me know in the comments which factoid on folate from this article you found most interesting — or, if you had more than one, share your favorites! There’s a lot to absorb (pun intended).
Until next time,
Lily
PS – If you like this type of in-depth information, you’ll love Real Food for Pregnancy. Check it out here or grab the first chapter for free (see below or the freebies page).
Knowledge is power. Empower yourself to have the healthiest pregnancy possible. Whether you’re thinking about getting pregnant or are 39 weeks along, there’s never a bad time to implement a nutrient-dense, real food diet.
PPS – Do you still have unanswered questions about folate? Since this article was originally published, I received so many requests for more detailed information that we created an entire 2-hour webinar covering folate metabolism & methylation at a deeper level with a specific focus on how this affects affects fertility and pregnancy outcomes. If you want more information about:
- folate absorption & metabolic pathways
- understanding the different forms of folate and how they behave in the body
- detailed information on MTHFR and the many MTHFR variations (which ones affect fertility and which ones have a negligible impact)
- the research on folic acid & autism
- folate and sperm health
- consequences of unmetabolized folic acid
- interpreting lab values (how much folate is too much & how do you accurately assess folate status & methylation?)
- medications and factors that may contribute to folate deficiency
- and so much more…
Check out our on-demand folate webinar co-taught by myself (Lily Nichols) and my dietitian colleague, Ayla Barmmer. We cover dozens of additional research papers not included in this article. Details here: Folate & Methylation in Fertility & Pregnancy
References
- Obeid, Rima, Wolfgang Holzgreve, and Klaus Pietrzik. “Folate supplementation for prevention of congenital heart defects and low birth weight: an update.” Cardiovascular diagnosis and therapy 9.Suppl 2 (2019): S424.
- Kirsch, Susanne H., et al. “Assay of whole blood (6S)-5-CH 3-H 4 folate using ultra performance liquid chromatography tandem mass spectrometry.” Analytical and bioanalytical chemistry 404.3 (2012): 895-902.
- Ferrazzi, Enrico, Giulia Tiso, and Daniela Di Martino. “Folic acid versus 5-methyl tetrahydrofolate supplementation in pregnancy.” European Journal of Obstetrics & Gynecology and Reproductive Biology (2020).
- U.S. National Library of Medicine. Genetics Home Reference: MTHFR Gene. https://ghr.nlm.nih.gov/gene/MTHFR#conditions
- Obeid, Rima, Wolfgang Holzgreve, and Klaus Pietrzik. “Is 5-methyltetrahydrofolate an alternative to folic acid for the prevention of neural tube defects?.” Journal of perinatal medicine 41.5 (2013): 469-483.
- Bailey, Regan L., et al. “Correspondence of folate dietary intake and biomarker data.” The American Journal of Clinical Nutrition 105.6 (2017): 1336-1343.
- Branum AM, Bailey R, Singer BJ. Dietary supplement use and folate status during pregnancy in the United States. Journal of Nutrition 2013; 143:486–492.
- Cornet, Dominique, et al. “High doses of folic acid induce a pseudo-methylenetetrahydrofolate syndrome.” SAGE open medical case reports 7 (2019): 2050313X19850435.
- Smith, A. David, Young-In Kim, and Helga Refsum. “Is folic acid good for everyone?.” The American journal of clinical nutrition 87.3 (2008): 517-533.
- Cavallé-Busquets, Pere, et al. “Moderately elevated first trimester fasting plasma total homocysteine is associated with increased probability of miscarriage. The Reus-Tarragona Birth Cohort Study.” Biochimie (2020).
- Quere, Isabelle, et al. “A woman with five consecutive fetal deaths: case report and retrospective analysis of hyperhomocysteinemia prevalence in 100 consecutive women with recurrent miscarriages.” Fertility and sterility 69.1 (1998): 152-154.
- Unfried, Gertrud, et al. “The C677T polymorphism of the methylenetetrahydrofolate reductase gene and idiopathic recurrent miscarriage.” Obstetrics & Gynecology 99.4 (2002): 614-619.
- Nelen, Willianne LDM, et al. “Maternal homocysteine and chorionic vascularization in recurrent early pregnancy loss.” Human Reproduction 15.4 (2000): 954-960.
- Abd Al-Badri, Hadeel J., and Miami Abdul-Hassan. “Serum total homocysteine level in Iraqi woman with unexplained recurrent miscarriage.” JPMA. The Journal of the Pakistan Medical Association 69.8 (2019): S26.
- Recber, Tuba, et al. “Metabolic infrastructure of pregnant women with methylenetetrahydrofolate reductase polymorphisms: A metabolomic analysis.” Biomedical Chromatography (2020): e4842.
- Serapinas, Danielius, et al. “The importance of folate, vitamins B6 and B12 for the lowering of homocysteine concentrations for patients with recurrent pregnancy loss and MTHFR mutations.” Reproductive Toxicology 72 (2017): 159-163.
- Aarabi, Mahmoud, et al. “High-dose folic acid supplementation alters the human sperm methylome and is influenced by the MTHFR C677T polymorphism.” Human molecular genetics 24.22 (2015): 6301-6313.
- Aarabi, Mahmoud, et al. “Testicular MTHFR deficiency may explain sperm DNA hypomethylation associated with high dose folic acid supplementation.” Human molecular genetics 27.7 (2018): 1123-1135.
- Bailey, Steven W., and June E. Ayling. “The pharmacokinetic advantage of 5-methyltetrahydrofolate for minimization of the risk for birth defects.” Scientific reports 8.1 (2018): 4096.
- Sweeney, Mary R., et al. “Evidence of unmetabolised folic acid in cord blood of newborn and serum of 4-day-old infants.” British Journal of Nutrition 94.5 (2005): 727-730.
- Plumptre, Lesley, et al. “High concentrations of folate and unmetabolized folic acid in a cohort of pregnant Canadian women and umbilical cord blood.” The American journal of clinical nutrition 102.4 (2015): 848-857.
- Niknamian, Soroush, and Somayeh Zaminpira. “Synthetic Folic Acid Supplementation during Pregnancy Increases the Risk of Neonatal Jaundice in Newborns.” JMEST 3.12 (2016): 6429-6431.
- Yang, Liu, et al. “High dose of maternal folic acid supplementation is associated to infant asthma.” Food and Chemical Toxicology 75 (2015): 88-93.
- Wiens, Darrell, and M. Catherine DeSoto. “Is high folic acid intake a risk factor for autism?—a review.” Brain sciences 7.11 (2017): 149.
- Tan, Mei, et al. “Maternal folic acid and micronutrient supplementation is associated with vitamin levels and symptoms in children with autism spectrum disorders.” Reproductive Toxicology 91 (2020): 109-115.
- Levine, Stephen Z., et al. “Association of maternal use of folic acid and multivitamin supplements in the periods before and during pregnancy with the risk of autism spectrum disorder in offspring.” JAMA psychiatry 75.2 (2018): 176-184.
- Friel, C., et al. “OP92 Does maternal folic acid supplements in pregnancy influence autism spectrum disorder in children? A systematic review and meta-analysis.” (2020): A43-A43.
- Valera-Gran, Desirée, et al. “Folic acid supplements during pregnancy and child psychomotor development after the first year of life.” JAMA pediatrics 168.11 (2014): e142611-e142611.
- Valera-Gran, Desirée, et al. “Effect of maternal high dosages of folic acid supplements on neurocognitive development in children at 4–5 y of age: the prospective birth cohort Infancia y Medio Ambiente (INMA) study.” The American Journal of Clinical Nutrition 106.3 (2017): 878-887.
- Kapoor, Vishal, et al. “Frenotomy for tongue-tie in Australian children, 2006–2016: An increasing problem.” The Medical Journal of Australia 208.2 (2018): 88-89.
- Walsh J, Links A, Boss E, Tunkel D. Ankyloglossia and lingual frenotomy: national trends in inpatient diagnosis and management in the United States, 1997–2012. Otolaryngol Head Neck Surg 2017; 156: 735-740.
- Joseph KS, Kinniburg B, Metcalfe A, et al. Temporal trends in ankyloglossia and frenotomy in British Columbia, Canada, 2004–2013: a population-based study. CMAJ Open 2016; 4: e33-e40.
- Amitai, Yona, et al. “Pre-conceptional folic acid supplementation: A possible cause for the increasing rates of ankyloglossia.” Medical Hypotheses 134 (2020): 109508.
- Czarnowska, Marta, and Elzbieta Gujska. “Effect of freezing technology and storage conditions on folate content in selected vegetables.” Plant foods for human nutrition 67.4 (2012): 401-406.



Thank you for this! I have had a hard time remembering which is better on the back of prenatal vitamins (should I be looking for folate or folic acid?) and this article hammered it home for me that folic acid is the manmade version.
As always, your essays encourage me to keep eating real food with the understanding of the nutrients and why they are important.
Yes, real food first and foremost!
This is incredible information in a way that’s easy to understand- thank you thank you!!
Glad it was coherent, albeit long!
Not folate/folic acid related. But my husband regularly ate brazil nuts for the selenium. However, he recently learned that the level of selenium in brazil nuts can vary from 0, to off the charts, depending on how and where they are grown. And he doesn’t know of a good way to find out what the selenium content of the nuts he’s eating are. Since you are my go-to expert on nutrition, I was wondering if you had come across this before, and had any insight about what the best sources of selenium are, or if there are certain brands of brazil nuts that are trustworthy. TY.
Hi Lily, fantastic read, I love the correlation between folate lowering homocysteine and therefore lowering the chance of miscarrying as well as other pregnancy and birthing problems. I don’t think the importance of homocysteine levels are talked about enough so I’m glad to see it written about here.
I agree. Homocysteine levels are so commonly overlooked!
I finally got a chance to read this. Was very interested because I was thankfully advised by the naturopath about the need to focus on folate over folic acid when I was trying to conceive a couple years ago. My now 11 month old daughter still ended up with a slight posterior tongue tie though, so I will be interested to see how the research into that possible link develops.
What really struck me about this brief was the amounts of folic acid in processed foods. Years ago I was having fertility challenges (and pain, weight, hunger, reproductive cycle issues) up until I stopped eating wheat. I’m not sure if I’m celiac but I wonder if some of us are super sensitive to all the crap that is pumped into processed and fortified foods. Maybe the residue of the folic acid was enough to cause my daughters tie.
On a side note, I heard about you on the Birthful podcast during my first trimester and was glad I got your book then because I ended up having gestational diabetes. I had a very healthy pregnancy, a natural delivery, a fantastic recovery, and seem to have a healthy baby (minus the tongue tie). I know I owe a lot of this to you.
Thank you so much for what you do and for making the main points of your findings free!
Excellent article and very well researched. Thank you so much for providing this content for free! I recommend your book to everyone I know — it has helped me immensely!
Thank you so much!
Hi Lily, this drives the point home to me that real food is really the best way to go, rather than trying to discern the “golden groupings” of nutrients in a pill (e.g. choline with folate, with B12, and in what ratios). I have the MTHFR mutation, and I’ve always wondered whether it affects just folic acid intake or also food folate (or methylfolate in a pill). I’ve added liver to my diet and just cooked pancreas (!), trying to be simple and as close to the source as possible
Yes, the more research I do, the more I come back to the amazing wisdom within real food.
What stood out to me was the potential dangers of taking large doses of folic acid prior to and during pregnancy. When I was young and unhealthy due to very poor childhood and adolescent nutrition, among other factors, I had an unplanned pregnancy with a lethal neural tube defect. The next pregnancy I had, I was told to take a very large dose of folic acid. I think I took it a few times but stopped, and I also couldn’t bring myself to regularly take my prenatal vitamins that pregnancy (which contained folic acid). I wonder if that was due to my body’s innate wisdom. Even as recently as 2016 a nurse midwife offhandedly mentioned that I should be taking a massive dose of folic acid prior to conception and during pregnancy due to my history. I am so glad that I know better now and can better educate my patients and friends, too! Thank you for this great article and your book. I recommend it all the time.
At a preconception appointment with a senior MFM, a MTHFR variant was discovered in my testing. I said “ok, I will make sure I take Methylfolate”. She screwed up her face, said No! very loudly and instructed me to double my folic acid intake. That was the moment I decided she would form no part of my prenatal care team.
Oh my, that’s disappointing!
Thank you so much for such an awesome research. I Love your book, Real food for pregnancy. It’s the only pregnancy book that I need to read.
Could you please recommend prenatal vitamins for men?
Thank you!
Thank you for another easy to understand, research backed article!
I took a methylfolate capsule by Jarrow when trying to conceive and throughout my pregnancy. I have stopped taking it while breastfeeding. Should I continue to take it? Should I resume taking it when TTC our 2nd child or just continue to eat a diet rich in folate (I love eggs, nuts and spinach!)?
PS. My son had a tongue tie corrected at the hospital right after birth. I take Rainbow Light prenatal vitamins. I am certain they contain folic acid.
Hi Lily, phew you put so much work in this! Thank you!
I wonder if my understanding is correct please – I currently use a basic prenatal with 400mcg folic acid; could I buy and take an additional supplement of L-methylfolate (400mcg too) and keep taking both? I understand that adding the natural form won’t harm.
My main issue here is budget. And recreating my own assortment seems difficult to do, so I am exploring this option.
I am in week 8.
Thank you very much!
This article was so well thought out and a great resource for the average person or the professional. Thank you for taking your time creating such an amazing resource.
Glad it was helpful. These articles are a labor of love, that’s for sure. Many dozens of hours go into each one. 🙂
Such an interesting article, thank you Lily.
I found the part on increasing rates of frenotomy fascinating (I am noticing this is quite common among friends babies). And I appreciate your pre-natal vitamin suggestions – pleased to see the one I take is on that shortlist!
Thanks Scarlett!
Wow amazing article, all your hard work put in this is much appreciated!
I’m #ttc and currently having 400 mcg folic acid in supplement and eat real food w loads of eggs, spinach, etc etc. The two recommended prenatals are not available in Europe. Any recommendation what to do?
Thanks so much
Seeking Health has European distributors. Check their website.
Super informative article! I’ve been trying to figure out for several days which prenatals are best.
I stopped on Seeking health but the concentration of some vitamins is very high.
For example vit B12 has a concentration of 150mcg and in another article of yours it says that the daily dose for a pregnant woman is 2.6mcg.
I would really appreciate it if you could give me an answer!
Thanks in advance!
Since B12 is challenging to absorb, it’s very common to include higher doses in supplements. This is pretty low risk as well, since it’s water soluble and excess is excreted in urine.
Thank you so much for taking the time to write this article. Back in December I found out that my daughter had anencephaly and since her death I have been doing a ton of research on folate. This article does such a great job of explaining everything and I love that you include all the references. I am also so grateful that you mentioned choline and the impact it might have on pregnancy. I’m definitely going to share this article with the other moms. I can’t wait to read more of your articles and finish your book. Thanks again for getting this information out.
I’m so very sorry for your loss. <3
This is great. Thanks for the long read and for including this source list. I’m 8 weeks along and I’ve already blasted through your book. My doctor gave me the exact response you address above when I said I was taking l-methylfolate. This post helps me to feel confident enough to have more informed conversations with her to explain why I’m taking folate rather than folic acid.
As a side note…your chapter on lab tests inspired me to request additional bloodwork, and not just go along with the default blood panel recommended. Hello additional vitamin D and thyroid checks pls!
Wow that’s a lot of info and research!
I decided to check my prenatal, it has folate as L-5-Methyltetrahydrofolate, 1.7mg DFE. What does that mean? Is that adequate?
Thank you very much for this excellently written and comprehensive article! Your book and articles are my go-to resources for everything pregnancy-related.
Happy to hear that, Anne!
Wow! What a power packed post! I am a homebirth nurse midwife and recommend your website and books to all. Best message for me here is that folic acid can impair folate absorption/metabolism. I had no idea. Thank you so much!
Curious how important folate is in a methionine rich diet… Based on this article I understand that our need for folate is to convert homocysteine to methionine, but the amino acid methionine is very easy to consume directly from foods.
What am I missing?
This would only make sense if the only role of folate in the body is for that one biological process. That is not the case!
Hi Lily. I hope I didn’t miss the answer to this question already–but can one take TOO much methylfolate? If I am taking it in a prenatal and also focusing on folate-rich foods will I get too much or will my body simply excrete the excess? Thank you!!
I don’t recommend exceeding the upper limit of 1,000 mcg/day. There are too many unknowns. Support methylation and the folate cycle with the full spectrum of complementary nutrients instead of mega dosing.
Hi Lily,
This is the big question in my head. So I am ready to purchase Optimal Prenatal it seems great, but I am also changing my diet a little further to be able to get most of my nutrients from food and just using the prenatal vitamins as umbrella insurance (as advised by your book). My worry is: This prenatal vitamin comes with 1360 mcg DFE – is it dangerous? Could it be too much, especially when combined with a nutritious diet?
Dietary folate equivalents (DFE) are complicated. It’s a topic we go into in our folate webinar in more detail. 1360 mcg DFE is actually equivalent to 800 mcg. Not too high. Not dangerous whatsoever. There is no upper limit for methylfolate, only for folic acid.
Thank you for this, really informative! I took folate during the beginning of my pregnancy, no folic acid or foods fortified with it, but my daughter unfortunately still ended up with a tongue and lip tie. I’m really wondering why that happened.
Aren’t tongue and lip ties largely genetic? I’ve also read that there may be a link between them and Vitamin A deficiencies.
Amazing insights! Thanks for explaining the difference between supplemental or fortified folic acid and natural folate in foods. I saw that my prenatal vitamin has both folic acid (400ug) and folate (416ug). I’m an American living in Germany so the vitamin label is in German, but I think the L-Methylfolate is the good stuff 🙂
I also eat a lot of greens and nuts (not much liver) and my recent bloodwork showed folic acid results (folsaure in German) showed 40ng, which I think they told me is high. After reading this article I’m hoping that doesn’t mean I might have unmetabolized folic acid. Any thoughts on what additional bloodwork I could ask for to check this?
I love your Real Food for Pregnancy book! I’ve read it all the way through once and many chapters for a second or third time 🙂
I so appreciate your ability to translate what seem like complicated nutrition and biochemical science into concepts that are understandable, as well as provide practical and actionable steps. As a senior in an undergraduate dietetics program, I always enjoy your insight and your courage to use the research to challenge the conventional prenatal nutrition wisdom. I look forward to being able to do this in my future career as an RDN! This post inspired me to do a final research paper on folate vs. folic acid, and I have downloaded all of the papers you cited – thank you!
Good work! Feel free to share with us via email (see our contact page) when it’s completed.
Can you please recommend some prenatal you find to be comprehensive for a woman/babies needs?
There are two linked right here in the article. <3
Should I choose a wholefood prenatal over synthetic? Because even though full circle and seeking health are recommended, aren’t they still lab made and not wholefood? Should moms try to find a wholefood prenatal w folate instead???
I love your blog and your well researched attitude toward current trends in nutrition. I was desperately looking for something this well reasoned and well put together. Sadly, I found out about your work only after my child turned 2 years old. So I did not benefit from this knowledge while pregnant. But, I do work with pregnant women and will recommend this website as a resource for sure.
My 30-week CBC came back with below-range lymphocytes, below-range erythrocytes, above-range MCV, and above-range MCH. Doc says it is probably B12 or folate deficiency (vs. anemia). But my prenatal I just started a week or so ago has 1360mcg of real folate and 2.6mcg of B12. The ones before that, 800mcg folic acid and 500mcg B12. Better to just eat some liver or add in some B12 drops?
We’re not able to give medical/nutritional advice in this format. If you’ve read Real Food for Pregnancy, you may recall the note of studies showing B12 requirements in pregnancy are actually 3x higher than current recommendations. Definitely follow up with your provider on this for additional testing and/or treatment advice.
Lily thank you for this informative article. Can you tell us what dosage of L-methylfolate pregnant women with the MTHFR mutation should be taking?
Hi Lily, Thank you for this informative article. Can you please tell us what dosage of L-methylfolate pregnant women should take? If you have any recommended brands that would be great as well.
A link to recommended brands is her book! 🙂
Above she says 600 mcg for pregnant women, 400 much for not (TTC?).
400 much = 400 mcg
Thank you for the information! The part on tongue tie is particularly intriguing since my babies struggled with it. I hope you’ll post any new research that comes up.
Hi Lily, thank you for the article. Please let me know if I undetstud this right Theres a limit of 1000 mcg of folic acid, but no limit of Folate? . I’m taking 800mcg in prenatal, + 400 mcg in my Calcium suplement. Please help me, if this is ok or too much.
What is a healthy folate level in the blood (TTC)? I have been taking 333 mcg of L-5-Methyltetrahydrofolic acid, glucosamine salt daily for 2 months and just got my blood panel back with 45.4 nmol/L Folate and the reference is given as 8.7 nmol/L so I’m well above recommend, but is it to low for TTC or too high? Thanks!
Blood levels of folate are covered in our practitioner webinar on folate. We’re not able to offer medical advice in this format. https://whnacademy.com/product/folate/
Hi Lily, could you please tell me if 5-methyltetrahydrofolic acid is the same as 5-MTHF? I am slightly confused about the ending „folic acid „… And would quadrefolic be an interesting option?
Those are all the same thing going by different names. I link to an article within this post explaining all of those from Dr. Ben Lynch.
Hi Lily!
Thanks so much for the work you’ve done/do on prenatal nutrition! I wanted to get your take on optimal blood folate levels. I just got mine tested and after taking methyl folate for the last 3 months my folate levels were above 20 nanograms per milliliter. I was curious what the optimal levels are, if you can take too much methyl folate, and which type of blood test would be best for us to determine that?
Thank you!
We cover the ins and outs of lab testing folate status in the Folate & Methylation in Fertility and Pregnancy webinar, available on demand here: https://whnacademy.com/product/folate/
Hi Lily,
What are your thoughts on folate-rich foods (especially leafy greens) losing a significant portion of their folate content just by “sitting around”? I was recently shocked to discover that some studies have found that spinach, for example, loses 50% of its folate after 8 days in the fridge (?!) (in addition to most of the vitamin C)….. room temperature was even worse. So realistically, if I buy spinach from the grocery store, it is probably already at least a week old, and combine that with a week that it spends in my fridge (if I eat a little bit every day), I wonder how much folate I am really getting from it?? I know you mentioned that freezing reduces folate a bit, but it kind of sounds like it might be a better option than eating spinach stored in the fridge…..?
Thanks!
Yes, this is true. I go into more detail on all the ways folate can degrade from foods in my folate webinar. https://whnacademy.com/product/folate/ Animal foods seem to be more resistant to folate degradation relative to plant foods. If possible, the sooner you eat your food after harvest, the better. It’s a good reason to try to connect with local growers (such as purchasing at the farmers’ market or try your hand at growing your own — spinach and many greens are super easy to grow!).
In my country, pregnant women are prescribed 5mg folic acid daily. Our pharmacies only carry 5mg/tablet folic acid…
Hi Lily,
It is very well informed! I love your book too!
I regurarly have bloodwork. For my folate serum;
In 2020, it was 9,03 ng/ml
In 2021, it was 13,21 mg/ml (I ate more livers than in 2019)
I don’t take folate/folic acid supplement and no fortified food as you mentioned above. I mostly do keto lifestyle.
Question: is it OK to skip folate supplement since my folate blood serum is sufficient (above 4ng/ml)?
That’s beyond the scope of something I can answer outside of a formal client-dietitian relationship, however we do cover folate bloodwork in the folate & methylation webinar.
Hi Lily. Do you have another recommendation for at home testing of MTHFR? The link in your article doesn’t work anymore. Thank you!
Looks like the link changed. I’ll update it in the post, but I’ll put it here as well for quick reference: MTHFR home testing.
Hi!
What is the RDA for methyl-folate if you DON’T have the genetic mutation? Is 400-600mcg still considered adequate? From my understanding the recommendation for 400mcg is based on folic acid supplementation – not methyl-folate. Any resources/info you have on this would be super useful!
The RDA makes zero consideration of genetics, so you can apply the 400-600 mcg across the board. Certainly someone with no MTHFR issues should be fine with the RDA level.
Hi Lily,
Thanks for this article. I also have your book and have followed it for my pregnancies. Curious if you have found any information on the anti-folate properties of tea? I have read a few journal articles and it seems like it is very dose dependent, but still a little scary!
Yes, tea consumption can impair bioavailability of folate, but that appears to be only when intake is >3 cups/day. Interestingly, aversions to tea are quite common in early pregnancy and it’s possible that this could be one reason why.
Reference: Yazdy, Mahsa M et al. “Maternal tea consumption during early pregnancy and the risk of spina bifida.” Birth defects research. Part A, Clinical and molecular teratology vol. 94,10 (2012): 756-61. doi:10.1002/bdra.23025
Yes, that’s one I read as well. It seems like matcha could be problematic at lower servings given its higher concentration of EGCG.
Wow this was a great read. Something I’ve been aware of, as I was tested for MTHFR years ago, but haven’t know much indepth.
Here in NZ any women with a higher than normal BMI is prescribed 5,000mcg of folic acid, which is taken in addition to whatever prenatal they’re on (Elevit is the blanket recommended here). Our table salt and all non organic wheat flour and products made with those items are legally required to be pumped with folic acid too. I can only imagine how much we are getting.