Vitamin D and Pregnancy: Why it matters, why deficiency is common, and how to ensure you’re getting enough
Many people are familiar with the role of vitamin D in bone health, but the function of this nutrient extends far beyond this. During pregnancy, vitamin D is crucial for many aspects of maternal and fetal health.
Research from the past 20 years has exploded on this topic, indicating that having sufficient vitamin D levels can reduce the risk of numerous pregnancy complications and promote optimal fetal development, and yet updates to official recommendations are lagging.
This article will discuss the importance of vitamin D in pregnancy, how much of this nutrient is needed during this stage of life, and how this compares to current recommendations.
What are the functions of vitamin D?
Although called a ‘vitamin’, vitamin D would actually be better classified as a hormone. It performs a variety of functions, including maintenance of normal blood levels of calcium and phosphorus and the promotion of bone, cardiovascular, endocrine, neural, and immune health, just to name a few.
This nutrient regulates fully 3% of the human genome — more than any other single nutrient.
Why is vitamin D important during pregnancy?
A better question might be: Why has it taken so long for us to recognize the many ways vitamin D is important during pregnancy?
This nutrient is involved in numerous processes within the body that ensure a healthy pregnancy, including:
- Aiding implantation
- Supporting fetal growth and skeletal development
- Regulating placental function & placental hormone levels
- Limiting production of proinflammatory cytokines
- Regulating blood sugar and insulin levels
- Promoting maturation of fetal lungs
- Maintaining endothelial integrity/membrane stability (this is important for regulation of blood pressure, among other functions)
Research has shown that those who maintain adequate vitamin D levels during pregnancy have a lower risk of many pregnancy complications, including:
- Gestational diabetes
- Preeclampsia
- Preterm birth
- Bacterial vaginosis
- Small for gestational age babies
One of the most compelling findings is related to preterm birth. In one study, mothers with adequate blood levels of vitamin D had a 60% lower risk of preterm birth. This finding held true even after adjusting for many confounding factors, including race. In women of color, the reduced risk of preterm birth was a shocking 78%. You can learn more about this study in one of my research briefs on Instagram.⠀⠀
Maternal vitamin D levels impact baby’s vitamin D levels
In addition to the effect on maternal well-being and birth outcomes, a mother’s vitamin D levels directly affect baby’s vitamin D levels since vitamin D is passed via the placenta (and after birth, via breast milk).
The consequences of low maternal vitamin D on the baby include: low birth weight, hypocalcemia (low blood calcium levels), and poor growth after birth. Additionally, a vitamin D deficiency during pregnancy can have long-term effects extending into adulthood, including dental enamel defects (leading to increased rates of cavities and dental issues), lower bone density (leading to higher rates of fractures), and even autoimmune diseases.
Yes, it can permanently affect your child’s bone development to include their teeth. In a 2019 well-designed double-blind, randomized controlled trial published in the Journal of the American Medical Association, researchers found that children of mothers supplemented with a higher dose of vitamin D (more than three times higher than the current recommended intake) in the third trimester had a 50% lower incidence of enamel defects as measured at age 6-years old. These are referred to as “dental enamel defects of developmental origin,” because they begin in utero and are apparent when the tooth first erupts. This type of enamel defect impacts 38% of children and prior to this research, there was no known predisposing factor.
The researchers wrote that these findings on vitamin D “indicate a breakthrough in understanding and prevention of the disease.”
How common is vitamin D deficiency in pregnancy?
Vitamin D deficiency in pregnancy is extremely common.
Vitamin D deficiency is prevalent throughout the world and in some places, affects up to 95% of pregnant women. There are many factors that influence your risk of vitamin D deficiency, including skin color, where you live in the world (especially the latitude), use of sunscreen, and a number of other factors, which I discuss below.
One of the major factors behind the current epidemic of vitamin D deficiency (there are many!) is a shift in our lifestyles away from time spent outside in the sunlight (without sunscreen) to indoor work and activities. When people do spend time outdoors, it’s often not at the time of day when the sun’s rays have the maximum potential to make vitamin D in your skin and/or people are covered up with sunscreen.
This is very different from our relationship with the outdoors and sun exposure even 50 or 100 years ago.
How do I know if I’m deficient in vitamin D during pregnancy?⠀⠀
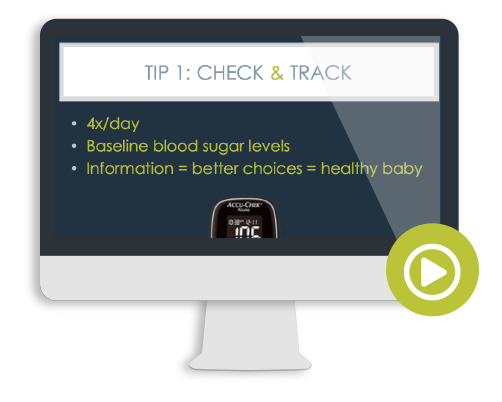
Screening for vitamin D deficiency is done with a blood test for the major circulating form of the nutrient (also called the storage form) known as 25-hydroxy-vitamin D.
Various organizations have different thresholds for what they consider “deficiency” or “insufficiency.” To keep it simple for the purposes of this article, I consider the bare minimum level to be 30 ng/ml.***
There’s growing research to suggest a minimum of 40 ng/ml is even better. The research study that found a 60% reduced risk of preterm birth in women with sufficient vitamin D levels found that a threshold of 40 ng/ml was needed for maximal reduction in preterm birth rates.
Finally, there are some vitamin D researchers who suggest even higher levels, often in the 50-80 ng/ml range, although research specific to pregnancy using those reference ranges is lacking.
Therefore, until there is more research, I generally default to a goal of 40 ng/ml.
This is right in line with the natural vitamin D levels observed in free-living hunter gatherer populations in Africa.
My opinion is: when in doubt, err for what is physiologically normal among humans living as close to our ancestral roots as possible.
For more detailed information, I cover all of these divergent opinions on serum vitamin D levels in my webinar on vitamin D & pregnancy.
***NOTE: Vitamin D can be reported in different units depending on your country: ng/ml or nmol/L. One very common error in interpreting vitamin D research and lab results is not checking the units. The unit conversion 1 ng/ml = 2.5 nmol/L, so the bare minimum goal of 30 ng/ml translates to 75 nmol/L. Always, always, always check your units.
Different forms of vitamin D: the devil’s in the details
Keep in mind when checking vitamin D levels that there are different forms you can measure in the blood. Since vitamin D functions like a hormone within the body, your body can “activate” stored vitamin D into its hormonally active form when needed (assuming you have enough vitamin D stored up, that is).
After you consume vitamin D from food (or supplements) or manufacture vitamin D from sunlight, your body converts this form (vitamin D3) into a circulating form known as 25-hydroxy-vitamin D, often written in shorthand as 25 (OH) D. This is the form of vitamin D that most lab tests assess when they check your vitamin D status. Your body maintains these levels for several weeks.
As needed, your body “activates” this form into 1,25 (OH)2D, which is also called calcitriol. Calcitriol is the hormonally active form of vitamin D. This sticks around in your bloodstream for hours (usually less than half a day), so it fluctuates quite a bit. It is not routinely screened for unless your care team suspects a defect in your body’s ability to convert vitamin D.
There is no other time in our lifespan other than pregnancy where the body activates more vitamin D. In fact, during pregnancy, levels of this “activated” form of vitamin D (calcitriol) rise immediately after conception and by 12 weeks gestation, are two to three times higher than baseline. Again, this is a hormonally-mediated process and it’s entirely normal.
Ensure that your provider is checking the correct form to assess your vitamin D status
Vitamin D metabolism changes drastically during pregnancy.
As pregnancy progresses, levels of activated vitamin D continue to rise, reaching what’s known as “supraphysiologic” levels.
Under any other condition, these extremely high levels of calcitriol would be concerning, but they are physiologically normal during pregnancy and play both direct and important roles in placental function, insulin resistance, regulating the genetic expression in your baby, promoting normal fetal bone development, and may even have long-lasting beneficial effects on a child’s future risk of disease, including lowering the risk of type 1 diabetes.
If your provider accidentally checks your levels of calcitriol instead of 25-hydroxy-vitamin D, (which is easy to do because the shorthand for calcitriol is 1-25-dihydroxy-vitamin D) — AND if they’re not familiar with the unusual metabolism of vitamin D in pregnancy — you’ll get a very dire warning from your provider that you have “toxic” levels of vitamin D when, in fact, your vitamin D metabolism is perfectly normal. I would know. This happened to me and I wrote about it here.
So again, make sure you spell it out for them, as not many providers have training on vitamin D, let alone vitamin D metabolism in pregnancy (if they took my webinar, this wouldn’t be a problem!).
How much vitamin D do you need during pregnancy? Is the current RDA for vitamin D enough?
Currently, the recommended daily allowance for vitamin D is set at 600 IU per day for pregnancy (that’s up from the previous recommendation of 400 IU).
This is unfortunate because numerous studies have shown that this amount is too low and consistently results in vitamin D deficiency, particularly in women of color (more on why this is the case below).
There have been several randomized controlled trials conducted on vitamin D supplementation in pregnant women to show that a number closer to 4,000 IU taken per day is not only safe, but optimal during pregnancy and that the current RDA of 600 IU is insufficient.
If you recall from my article “10 Things You Didn’t Know About Vitamin D,” vitamin D researchers have pointed out that the Institute of Medicine (IOM) likely underestimated vitamin D requirements by upwards of a factor of ten.
There are many studies to demonstrate that 4,000 IU is both a safe and effective dosage and also ideal for sustaining vitamin D metabolism during pregnancy.
Excuse the alphabet soup here, but it boils down to this… In order to maintain the “supraphysiological” levels of calcitriol (hormonally active vitamin D that is so crucial in pregnancy), we need to maintain sufficient 25-hydroxy-vitamin D (the substrate your body uses to produce calcitriol) and the research shows we need an intake of 4,000 IU of vitamin D at minimum to maintain enough 25-hydroxy vitamin D for this to happen.
As vitamin D researcher Dr. Bruce Hollis explains,
“While there has been considerable controversy surrounding the daily requirement of vitamin D and what constitutes sufficiency during these critical periods, there is mounting evidence of the importance of vitamin D supplementation during pregnancy to achieve a total circulating 25(OH)D concentration of a least 40 ng/mL, the point at which the conversion of 25(OH)D, the prehormone, to 1,25(OH)2D, the active hormone, is optimized and associated with a lower risk of comorbidities of pregnancy and better outcomes.”
This fact is well illustrated in the research. In one very well-designed double-blind, randomized controlled trial, pregnant women received 400, 2,000, or 4,000 IU of vitamin D3 per day starting between 12 and 16 weeks gestation until delivery. In the group that received the lowest dose (400 IU), only 50% of mothers had sufficient vitamin D levels at delivery (importantly, among the Black women in the trial, only 20% of them had sufficient vitamin D levels with the low 400 IU dosage).
In contrast, for women receiving the highest dose (4,000 IU), 82% had adequate vitamin D at delivery. In addition, adequate maternal vitamin D levels predicted newborn vitamin D levels (meaning higher dose supplementation significantly reduced the risk of newborn vitamin D deficiency). The researchers found no adverse events linked to the vitamin D supplementation and concluded that 4,000 IU per day for pregnant women is safe and was the most effective in achieving vitamin D sufficiency in all pregnant women and their newborns, regardless of race.
To drive the point home, the most recent Cochrane systematic review (systematic reviews are considered the king of all studies) on vitamin D in pregnancy showed that an amount of 4,000 IU is safe and that vitamin D supplementation probably reduces the risk of preeclampsia, gestational diabetes mellitus, having a low-birth weight baby and postpartum hemorrhage.
Several studies have used a dosage of 5,000 IU per day in pregnancy with positive outcomes and no adverse events (and others have used single very high dose interventions, again with no adverse events), however since these were not randomized, controlled trials, I continue to default to the 4,000 IU dosage as a baseline.
I’ve been writing and teaching about the importance of vitamin D for well over a decade now and it still shocks me that official recommendations have not been updated, and worse, that many providers caution against vitamin D supplementation despite zero evidence to back their claims of supposed danger.
Maybe I need to make bumper stickers that read: “4,000 IU of vitamin D/day in pregnancy is safe and effective!”
“But I heard that vitamin D supplementation can cause high blood calcium levels and calcification of tissues. Is that true? Can vitamin D supplementation in pregnancy be toxic?”
Good question! A number of the studies cited in this article (scroll down for a full reference list) have checked for precisely this. None of the clinical supplementation trials, including the ones using 4,000 and 5,000 IU, have had any cases of high blood calcium levels (hypercalcemia) at these dosages nor have they shown evidence of tissue calcification. Anyone claiming that this is the case has not been reading recent vitamin D research where randomized clinical trials have put these hypotheses to the test directly.
As always, vitamin D needs to be consumed along with synergistic nutrients to function optimally (explained in the next section, so keep reading!).
A few relevant quotes from one such trial showing 4,000 IU was superior to lower dosages:
“The only known avenue of vitamin D toxicity is manifested through hypercalcemia and hypercalciuria, neither of which was observed in our ramdomized, controlled trial (RCT). In fact, our Data and Safety Monitoring Committee concluded that not a single adverse event in this RCT could be attributed to vitamin D intake.”
And another, which also illustrates the unique shift in vitamin D metabolism during pregnancy that’s independent of calcium metabolism:
“From our data, it is evident that production of 1,25(OH)2D3 is really not under the control of the classic regulators of calcium, phosphorus, and PTH. The dramatic rise in maternal circulating 1,25(OH)2D3 following conception is remarkable for many reasons: By 12 weeks of gestation, maternal circulating 1,25(OH)2D3 levels are already triple those of a nonpregnant female. From that point in gestation, the 1,25(OH)2D3 levels rise much higher and are driven by substrate—25(OH)D—availability . This substrate dependence of 1,25(OH)2D3 production is never observed in normal human physiology driven by classic calcium homeostasis.
Another remarkable factor in pregnant women is how they can attain supraphysiologic levels of 1,25(OH)2D3, sometimes exceeding 700 pmol/L in our study, and never exhibit hypercalciuria or hypercalcemia. These tremendous circulating levels of 1,25(OH)2D3 during pregnancy are possibly of placental origin or from the renal 1‐α‐hydroxylase that would have to be uncoupled from feedback control and for reasons other than maintaining calcium homeostasis.”
As always, make sure to ask anyone making claims against vitamin D and pregnancy for research that support their conclusions. I am always open to changing my stance. In fact, I regularly search the medical journals for “[insert nutrient of concern] toxicity and pregnancy” to see if the research has evolved or if I need to adjust my recommendations to take into account new safety data.
Instead of supplementing with 4,000 IU, is there a way for me to get enough vitamin D through eating food alone?
I am always a proponent of food first; heck, my books specifically include “real food” in the title.
Unlike most nutrients, the major contributor to our intake is NOT food, it’s sunlight (or nowadays, supplements). In people who do not supplement, fully 90% of vitamin D status is attributed to what our bodies produce in our skin via sun exposure.
Even the richest dietary sources of vitamin D, namely fish liver or as the supplemental form cod liver oil, are not sufficient to meet vitamin D needs alone.
Other food sources of vitamin D have even lower concentrations. For example, many think that dairy products are a good source of vitamin D, and while they do contain some, it’s not enough as your sole source. An 8 oz glass of milk has only 100 IU of vitamin D on average.
When you consider the relatively low quantities of vitamin D in foods, it becomes clear that our bodies are designed to meet most of our vitamin D needs from sun exposure.
This doesn’t negate the importance of a well-balanced diet, however. Multiple nutrients work synergistically with vitamin D, including vitamin A, vitamin K2 (both of which are found in animal fats), magnesium, iron, calcium, zinc, copper, boron, among others.
I talk more about the specific amounts of vitamin D found naturally in foods in my webinar on vitamin D and pregnancy if you’re interested in learning more.
All in all, if you want to obtain adequate vitamin D without supplements, don’t look to food, look to sun exposure (and do become aware of the many factors that influence your vitamin D production from the sun; see the end of this article).
If regular sun exposure is not feasible for you, taking a supplement is an easy, affordable, and safe way you can ensure you are maintaining adequate levels of vitamin D.
I’m not partial to brands, but if your prenatal vitamin does not contain 4,000 IU (few do, although this is one exception), then I recommend a separate vitamin D supplement to make up the difference (again, unless you regularly get in the sun).
This is a solid product for a standalone vitamin D supplement with no questionable ingredients (it also has vitamin K2, which aids vitamin D metabolism).
If you look elsewhere for vitamin D supplements, ensure it is in the form of vitamin D3 (not vitamin D2), since vitamin D3 has been shown to sustain serum vitamin D levels for longer. Vitamin D3 is also the form that’s chemically identical to what your body obtains from food and produces from the sun.
Is 4,000 IU the right amount for everyone?
Although research suggests 4,000 IU likely provides a sufficient amount for pregnancy, there isn’t a “one-size-fits-all” when it comes to supplementation.
That’s because there are multiple factors that affect your ability to adequately synthesize or absorb vitamin D (more on that below).
A dose of 4,000 IU comes much closer to meeting your needs during pregnancy than the RDA of 600 IU, but there is still individual variation in vitamin D needs.
The only way to truly know whether you have an adequate vitamin D level is to test your 25-hydroxy-vitamin D serum level through a blood test. This can be ordered through your prenatal health care provider’s (or any physician’s) office.
For example, in both of my pregnancies, I lived in a northern latitude, where sufficient vitamin D production from sun exposure was impossible year-round. I needed more than 4,000 IU of supplemental vitamin D to maintain my serum levels despite consuming plenty of foods rich in vitamin D. I speak to the specifics in the Q&A portion at the end of my vitamin D & pregnancy webinar if you want the full details. Had I not measured my serum levels, I would never have known I needed more.
Previously, when I lived in a lower latitude (granted this was prior to pregnancy), I was able to maintain sufficient vitamin D levels through sun exposure alone. I specifically made it a priority to regularly schedule in sunbathing time (enough for vitamin D production, but not so much that I’d burn). This is why it’s so important to consider where you live when determining whether you’re at risk for deficiency and whether supplementation is right for you. It’s a tricky nutrient!
Factors that influence your risk of vitamin D deficiency
As alluded to earlier in this article, vitamin D deficiency is very common. The reasons for this are complex, so the following covers some factors that may affect your ability to obtain adequate vitamin D from sun exposure and/or are risk factors for deficiency. Hopefully this information can help you gauge how likely you are to be deficient.
- Skin color. Race and ethnicity are strong predictors of having a higher risk of vitamin D deficiency as measured by 25-hydroxy-vitamin D levels. Why? Because the pigment in our skin called melanin acts as a natural sunscreen and somewhat blocks UV-B rays from producing vitamin D in our skin. The more melanin in your skin, the more effective it is at blocking UV-B rays and thus vitamin D production. In fact, it’s been shown that Black people can require 6x more time in the sun to produce the same amount of vitamin D than people with pale skin, particularly in those who easily burn and freckle. Therefore, if you have dark skin, you typically have a higher risk of vitamin D deficiency and you will need a greater amount of time in the sun to produce sufficient vitamin D. This may explain at least one factor that contributes to racial disparities in pregnancy and birth outcomes for women of color. However, it’s reassuring to see that in studies where sufficient supplementation is provided to raise serum vitamin D levels, some of these adverse outcomes are ameliorated (recall the preterm birth study covered earlier in this article; that study provided vitamin D supplements in a dose of 5,000 IU/day). One simple but impactful way we can help reduce the racial disparity among pregnant women of color is to promote and ensure adequate vitamin D supplementation—and that means much more than 600 IU/day!
- Exposure to sunlight. Depending on your geographical location, age, skin color, and season, it can take more than four hours for your skin to synthesize sufficient vitamin D! Additionally, slathering on sunscreen causes a reduction in the skin’s capacity to produce vitamin D. A sunscreen with an SPF of 30 will absorb approximately 95-98% of solar UV-B radiation, which — no surprise — reduces the skin’s capacity to produce vitamin D by 95-98%. You’ve also probably heard that the sun is the strongest between the times of 10:00 AM to 2:00 PM; likewise, this time of day for outside exposure is also optimal for vitamin D synthesis since UV-B is at its maximum between these hours. You can use the app “D Minder” (no affiliation) to quantify how much vitamin D you make from the sun based on many different factors. It’s not perfect, but it gives a good “guesstimate.”
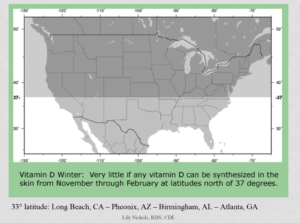
- Location. Where you live geographically can greatly affect your vitamin D levels. Pregnant women who reside at latitudes above the 37th parallel (see visual below to see where I’m talking about) are at an increased risk for deficiency, particularly during the winter and spring months, when you’re more likely to spend time inside. Even if you do go outside during these months, the time it can take to synthesize vitamin D via skin is very extensive. (Also, good luck laying out in a bikini in cold temps — brrrr!) So, if you reside north of the 37th parallel — the upper half of California, Nevada, Utah, Colorado, Kansas, Missouri, Kentucky, and Virginia — you are at risk for deficiency just from where you live alone. Some research suggests that the 33rd parallel be used instead, which means any people living above Los Angeles, CA to Atlanta, GA are at risk for deficiency in the winter; that’s most of the United States!
- Altitude. Those who live at lower elevations may be at greater risk for vitamin D deficiency because it takes a longer time for the solar UV-B to travel to the earth’s surface.
- Air pollution. Believe it or not, even the amount of pollution in the air is another factor that affects vitamin D levels. This is because high levels of atmospheric pollution can significantly reduce ground levels of UV-B, which will ultimately reduce ground levels of UV-B reaching your skin. If you live in a polluted city, you have a higher risk for vitamin D deficiency.
Do you see the common theme here? Pretty much anything that can “block” the sun from reaching your skin is a barrier that increases your risk for vitamin D deficiency.
- Season. The timing of your pregnancy can also have an impact on vitamin D levels for both you and your baby. In one cross-sectional study, researchers found that each season affected vitamin D serum concentrations; levels were the lowest in the month of January but then increased until the month of July. Similarly, in a cohort study, researchers found that season was the greatest factor associated with vitamin D insufficiency among pregnant women residing in the Southeast of the United States. While they did find that women with darker skin tones had a larger risk for vitamin D deficiency, they found that season had an even larger impact on vitamin D deficiency, even in the pregnant women with lighter skin tones. Consider your own pregnancy, will more than half of it be through the colder seasons (end of Fall, Winter, and early Spring)? If so, you have a much higher risk of vitamin D deficiency.
- BMI. Although the mechanism is not fully understood, low vitamin D levels have been found to be correlated with a BMI greater than 30. In addition, the higher a person’s BMI, the more likely they are to be deficient. Some research indicates that vitamin D can be sequestered into fatty tissue, making it unavailable to the body. Although BMI is not a direct measurement of a person’s body fat percentage, research has nonetheless shown it to be a useful factor in determining one’s risk for vitamin D deficiency. Therefore, if you begin pregnancy with a BMI greater than 30, make it a priority to ask your provider to screen for vitamin D deficiency. Some research suggests higher dose supplementation may be required in these individuals.
- Age. Aging has been found to reduce production of vitamin D synthesis in our skin. For example, a 70-year old’s skin has been found to only synthesize 25% the amount of vitamin D than that of a younger person.20 Aging affects the conversion of vitamin D into its active form. Production of calcitriol is reduced by 50% as a result of an age-related decline in kidney function. Obviously, our child-bearing age window doesn’t extend into our 70s, but it’s worth noting that the process of synthesizing vitamin D via our skin will continuously decline the older we get. On the flip side, some studies show that the younger maternal age has been associated with vitamin D deficiency. This may be due to other factors such as the fact that younger women may be more likely to perform shift work, which typically do not offer outside exposure during peak UV-B hours.
- Pre-existing medical conditions. There is evidence that vitamin D deficiency plays a possible role in numerous health problems such as cardiovascular disease, Parkinson’s disease, bone fractures, cancer, poor immune function, type 2 diabetes, depression, and autoimmune diseases, to name a few. It is possible that anyone with these conditions may have higher requirements for vitamin D; this is still debated in the literature. There are also certain medical conditions that may impair vitamin D absorption, which in turn may warrant an increase in vitamin D requirements. For example, because vitamin D is a fat-soluble vitamin, people with fat malabsorption disorders from conditions like liver disease, Cystic Fibrosis and Crohn’s disease may need higher vitamin D supplementation. Certain medications can also affect your vitamin D production and absorption, resulting in greater risk of deficiency. Discuss this possibility with your provider or pharmacist.
- Breastfeeding. If you are breastfeeding, vitamin D requirements are even higher than in pregnancy. There has even been research to define the amount of vitamin D needed to supply a sufficient amount of vitamin D for both the mother and infant, offering an alternative to vitamin D infant drops (details on vitamin D requirements during breastfeeding can be found in this post). If you are both pregnant and nursing, this may increase your vitamin D needs even more, though research on vitamin D needs for women who are both pregnant and breastfeeding is lacking.
Summary
All in all, vitamin D and pregnancy is an ever-expanding area of research. Some of the take home points here are that:
- Vitamin D deficiency is common for all of us, but especially during pregnancy
- Pregnancy induces significant changes in vitamin D metabolism, making it even more important for women to maintain sufficient intake
- Maternal vitamin D levels impact pregnancy outcomes, fetal/infant vitamin D levels, and may impact a child’s long-term health
- Vitamin D deficiency can be determined by a simple blood test; just ensure your provider orders the right one: 25-hydroxy vitamin D
- Sun exposure is the main determinant of vitamin D levels in those who do not supplement; food is tertiary
- Abundant research indicates that the current RDA for vitamin D is insufficient and instead, a baseline of 4,000 IU should be provided during pregnancy, with the amount adjusted per the client based on serum levels
- Numerous factors influence your risk of vitamin D deficiency; this nutrient/hormone is complex!
What do you think?
Now I’d love to hear from you in the comments below.
- What do you think about the recommendations for vitamin D during pregnancy compared to more current research?
- How much vitamin D does your prenatal multivitamin contain?
- Did your prenatal healthcare provider screen you for vitamin D deficiency and/or recommend supplementation?
Until next time,
Lily
PS – If you want more detailed information on vitamin D during pregnancy, be sure to check out my webinar: Everything You Need To Know About Vitamin D and Pregnancy. If you thought this post got into the weeds, this 90-minute webinar covers more than twice as many studies referenced in this article. This research-heavy presentation was specifically made for health practitioners, but all are welcome to attend. It’s available pre-recorded for on-demand viewing.
References
- Mulligan, Megan L., et al. “Implications of vitamin D deficiency in pregnancy and lactation.” American journal of obstetrics and gynecology 202.5 (2010): 429-e1.
- Palacios, Cristina, Lia K. Kostiuk, and Juan Pablo Peña‐Rosas. “Vitamin D supplementation for women during pregnancy.” Cochrane Database of Systematic Reviews 7 (2019).
- Wagner, Carol L et al. “A randomized trial of vitamin D supplementation in 2 community health center networks in South Carolina.” American Journal of Obstetrics and Gynecology vol. 208,2 (2013): 137.e1-13.
- Ingole, Jitendra, and Sonali Ingole. “Pregnancy and Vitamin D.” Journal of Mahatma Gandhi Institute of Medical Sciences 19.2 (2014): 89.
- Shin, Joong Sik, et al. “Vitamin D effects on pregnancy and the placenta.” Placenta 31.12 (2010): 1027-1034.
- McDonnell, Sharon L et al. “Maternal 25(OH)D concentrations ≥40 ng/mL associated with 60% lower preterm birth risk among general obstetrical patients at an urban medical center.” PloS one vol. 12,7 e0180483. 24 Jul. 2017.
- Al Emadi, Samar, and Mohammed Hammoudeh. “Vitamin D study in pregnant women and their babies.” Qatar medical journal 2013.1 (2013): 7.
- Schroth, Robert J., et al. “Prenatal vitamin D and dental caries in infants.” Pediatrics 133.5 (2014): e1277-e1284.
- Javaid, M. K., et al. “Maternal vitamin D status during pregnancy and childhood bone mass at age 9 years: a longitudinal study.” The Lancet 367.9504 (2006): 36-43.
- Nørrisgaard, Pia Elisabeth, et al. “Association of high-dose vitamin D supplementation during pregnancy with the risk of enamel defects in offspring: a 6-year follow-up of a randomized clinical trial.” JAMA pediatrics 173.10 (2019): 924-930.
- Pfotenhauer, Kim M., and Jay H. Shubrook. “Vitamin D deficiency, its role in health and disease, and current supplementation recommendations.” J Am Osteopath Assoc 117.5 (2017): 301-5.
- Bodnar, Lisa M., et al. “High prevalence of vitamin D insufficiency in black and white pregnant women residing in the northern United States and their neonates.” The Journal of nutrition 137.2 (2007): 447-452.
- Hollis, Bruce W., and Carol L. Wagner. “Vitamin D and pregnancy: skeletal effects, nonskeletal effects, and birth outcomes.” Calcified tissue international 92.2 (2013): 128-139.
- Hollis, Bruce W., and Carol L. Wagner. “New insights into the vitamin D requirements during pregnancy.” Bone research 5.1 (2017): 1-16.
- Hollis, Bruce W., and Carol L. Wagner. “Vitamin D requirements and supplementation during pregnancy.” Current Opinion in Endocrinology, Diabetes and Obesity 18.6 (2011): 371-375.
- Hollis, Bruce W., and Carol L. Wagner. “Vitamin D as a modifier of genomic function and phenotypic expression during pregnancy.” Molecular Nutrition: Mother and Infant. Academic Press, 2021. 361-399.
- Hollis, Bruce W et al. “Vitamin D supplementation during pregnancy: double-blind, randomized clinical trial of safety and effectiveness.” Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research vol. 26,10 (2011): 2341-57.
- Palacios, Cristina, Lia K. Kostiuk, and Juan Pablo Peña‐Rosas. “Vitamin D supplementation for women during pregnancy.” Cochrane Database of Systematic Reviews 7 (2019).
- Palacios, Cristina, et al. “Regimens of vitamin D supplementation for women during pregnancy.” Cochrane Database of Systematic Reviews 10 (2019).
- Oliveri, B., et al. “Vitamin D3 seems more appropriate than D2 to sustain adequate levels of 25OHD: a pharmacokinetic approach.” European journal of clinical nutrition 69.6 (2015): 697-702.
- Chawla, Devika, et al. “Racial and ethnic differences in predictors of vitamin D among pregnant women in south-eastern USA.” Journal of nutritional science 8 (2019).
- Gallagher, J. Christopher. “Vitamin D and aging.” Endocrinology and Metabolism Clinics 42.2 (2013): 319-332.
- Leary, Patrick F., et al. “Effect of latitude on vitamin D levels.” J Am Osteopath Assoc 117.7 (2017): 433-439.
- Schwalfenberg, Gerry. “Not enough vitamin D: health consequences for Canadians.” Canadian Family Physician 53.5 (2007): 841-854.
- Hosseinpanah, Farhad, et al. “The effects of air pollution on vitamin D status in healthy women: a cross sectional study.” BMC public health 10.1 (2010): 1-6.
- Scragg, Robert, and Carlos A. Camargo Jr. “Frequency of leisure-time physical activity and serum 25-hydroxyvitamin D levels in the US population: results from the Third National Health and Nutrition Examination Survey.” American journal of epidemiology 168.6 (2008): 577-586.
- Bischof, Martin G et al. “Vitamin D status and its relation to age and body mass index.” Hormone research vol. 66,5 (2006): 211-5.
- Delle Monache, Simona, et al. “Body mass index represents a good predictor of vitamin D status in women independently from age.” Clinical Nutrition 38.2 (2019): 829-834.
- Nair, Rathish, and Arun Maseeh. “Vitamin D: The “sunshine” vitamin.” Journal of pharmacology & pharmacotherapeutics 3.2 (2012): 118.
- Wagner, Carol L et al. “High-dose vitamin D3 supplementation in a cohort of breastfeeding mothers and their infants: a 6-month follow-up pilot study.” Breastfeeding medicine: the official journal of the Academy of Breastfeeding Medicine vol. 1,2 (2006): 59-70.




I’m currently 35wks pregnant and my provider never brought up vitamin D. But I was the one who brought it up at every visit up until about 28wks, I stopped testing it. Before pregnancy I was taking 4K/day and maintained levels in the 60s. First trimester at 8wks it went down in the 40s so I started taking 6k/day. Then the next test 4wks later was 122! So I quit all together and it went down to the 30s and my midwife said that was “normal” so I started taking 5k/day and haven’t checked it since. Each time I would request the labs they said there was no reason to keep checking it since it was normal the first time. And at the 24wk appt I want to say she told me there’s no need to keep checking it since the baby’s bones were already formed. I had to bite my tongue so hard! But they always ordered it when I asked and never said no.
Are you sure the measurement 4 weeks later was 25-hydroxy-vitamin D and not 1,25 dihydroxy vitamin D? That much of a jump is unlikely from 6k, but if they tested the wrong form, this would make sense. This is what happened to me. See the IG post I link within this article for the full story.
There are, of course, always individual variations. I recall from one study, there was one pregnant woman who had a large jump in her 25-hydroxy-vitamin D level from a 4k daily dosage, but that was only one out of hundreds in the study. So, it’s possible, but rare.
So my pcp actually screened me for vitamin D deficiency after I had an IUD removed and my period was slow to return. My OBGYN at the time never tested or brought it up. I did get pregnant and during the first trimester read your book so knew to ask my Midwife (changed providers) to test my vitamin D level again during the start of my third trimester just to make sure I was still on track. Had my baby almost two weeks ago and started upping my Vit D to 5000-6000IUs per day based on the evidence as I am exclusively breastfeeding and would like to avoid having to supplement baby with Vit D drops. See the pediatrician tomorrow and I know he is going to bring it up so interested to see what he says. I may ask for my level to be checked at my 6 week follow-up to confirm that my level is high enough for me and baby.
That’s great. A little bit of nuance though on breastfeeding… it’s not 25-hydroxy D that transfers through breast milk, it’s vitamin D3, which is why consistent intake on your part is so important (regardless of your serum 25 OH D). I talk about this more in this article. In other words, don’t skip the supplement (or sun exposure) because your serum levels are good. Make sense?
Going into my next round of IVF, and my REI tests for VitD every time. Thankfully with supplementation, I have been able to stay about 40!
That’s great. Thinking “sticky thoughts” for you, Larissa!
Hi Lily! I am so fascinated by the research contained in your books. I am not currently pregnant but was in 2018, and developed pre-eclampsia, starting with symptoms at 30 weeks. I went into my pregnancy with a Vitamin D deficiency (done through 25-hydroxy test with my PCP, 10 days before I found out was pregnant). I did not supplement because I couldn’t stomach an additional pill during the first trimester, and then just continued with my prenatal, which only had 600 iu of Vitamin D. I 100% believe that this deficiency along with others, caused me to have a complicated pregnancy. I delivered via c-section at 39+6, a thankfully healthy baby. I want to thank you for your information and continued research. It has made me think about and make lots of changes in my diet and supplementation for pregnancy next time, which I am hoping to be pregnant again in the next 1.5-2 years. I am hoping that with this knowledge and the changes I am making, that my experience will be entirely different. Thank you again for your wealth of knowledge!
You asked in your email if my GP ever screened for Vitamin D levels while pregnant – mine did not. However I asked for mine to checked, and it came back as an acceptable level – the accept level they had set – which was way below. So I increased my vitamin D and continued to check all through my own accord via iscreen – a site where I could order blood tests privately.
Yeah, the standard cut off is pretty low, with outright deficiency at <20 ng/ml. This is why it's helpful to look at the cut offs proposed by vitamin D researchers for "optimal" levels.
Hi there Lily,
Thanks for writing this article. When I was pregnant, I saw a research study on the wall of MSU about being pregnant and vitamin D level. I quickly read the discussion and saw it was important. I asked my doctor to get me tested and she said insurance will only pay for it if you “have low vitamin d levels” But she said it was silly because how would you ever know. Well I got tested and she tested the correct level and I had 17. She then told me how much vitamin D to take. I got tested 8 months postpartum and it was 27. I would love to get it up to 40 before I get pregnant again. Thank you for the reminder and all the information!
Lily,
As always thank you for such valuable information. My current prenatal (Ritual) has 2000IU. My provider did not test for Vitamin D deficiency, is it too late to start supplementing? I am currently 31 weeks.
It’s never too late to start! Especially if you’re planning on breastfeeding/feeding breastmilk, since the needs are higher then as well. 🙂
Thanks for all the great info. My doctor screened me for Vit D among other things in my12 week blood test. The recommended range was 32-100 ng/mL and I was low so she prescribed a supplement. I’ll be retested at 28 weeks. I’ve bumped up my daily supplementation in addition to the prescription so I hope that I’ve hit 40.
I should also note they suggest 1000-2000 iu per day once my levels are up. Sounds like they’re aiming a little low but not as bad as the standard recommendations.
I’m curious if you would recommend this for postpartum as well. Particularly curious about a possible link between Vitamin D deficiency and knee pain postpartum. Thoughts?
Yes it remains important postpartum, particularly if breastfeeding and the requirements are higher. See this post.
But I’d also look into nutrients to support connective tissue. See this article on postpartum recovery for more.
Thanks for this detail! My fertility doctor checked my vitamin D very early on but my gyno never did. I’m 19 weeks now. Do you recommend getting the D blood test multiple times throughout your pregnancy? I take a 2,000 IU supplement.
My OB office routinely checks 25-hydroxy, hemoglobin A1C, CBC, ferritin and possibly some others. They completed those labs earlier this week (during my 9th week) without me asking. They did for my first as well. My level 25-hydroxy level was 63 ng/mL and hemoglobin A1C was 4.6. My prenatal has 1,000iu but I’ve been taking an additional 5,000iu.
Thanks for the great info as always!!!!
Wow, they’re on top of it. Wonderful you found a proactive team!
I just love your articles, Lily!
I have requested my vitamin D levels to be monitored with my 3rd and 4th pregnancies. After giving birth to my second child, my level was 20!! Crazy low. And I felt awful. Also, she grew very slowly and walked and teethed very late, which I now believe was directly related to my D levels! I’m pretty sure my prenatal at that time only had 1000 IU. Now I take Full Circle Prenatal which has the full 4000 IU. However I will keep monitoring my levels with each trimester since I tend toward deficiency. I was able to get it up to 40 before conception, so I really hope that helps me and the baby to be much healthier.
Hi Lily,
I personally supplement as you have recommended. I have come across another provider previously which based on hair mineral analysis advises against vit d supplementation. As it seems to “decrease potassium and increase calcium” levels. Apparently throwing the thyroid out of balance. Do you know anything about this or whether it’s even an accurate form of measurement? I’m curious
My doctor never talked to me about vitamin D. I asked her during my 2nd pregnancy (I have 3 kids) if I could get my levels tested and I was told I could, but it wasn’t covered by insurance and would cost around $200. I decided not to do it. I wish I would have done more testing for each of my pregnancies to see where my nutrient levels were at. But thankfully I had 3 healthy pregnancies and births.
I am wondering how often during pregnancy you recommend having vitamin D testing done? Each trimester? Or more often than that? If it is low, long do you typically see it takes to increase in value?
It depends. I address lab testing in more detail in Ch 9 of Real Food for Pregnancy. If deficiency is present or a person is at risk, it makes sense to test each trimester to ensure levels are adequate. It often takes 1-2 months for serum values to reflect a change in supplementation.
Thank goodness for you Lily Nichols to provide us with this crucial information! We certainly aren’t getting it from our care providers! Never tested, never talked to about Vitamin D and pregnant with 2nd. My prenatal has 2000IU vitamin d3.
Thank you!!
I’m currently 29w pregnant with my second. My vit D status has always been followed in both pregnancies. With my son I was deficient and taking the highest UI supplement I could find (3000IE), but the levels never went up. I breastfed my son for two years and 1 year in I broke my foot. He also has 2 damaged teeth (a little corner broke off) without anyone being aware of an incident/fall.
This pregnancy I actually started with an ok-ish level! I was/am still supplementing with the same vit. D supplement + a cod liver oil supplement + more time spent outdoors. This seems to make all the difference. Despite being 5 years older and a BMI of 30 at conception I am so happy my vitamin D levels are a lot better than last time.
Hi Lily! I live in Kansas City, MO (latitude ~39 degrees N). I have been taking 4,000 IU of Vitamin D3 (via Full Circle) for the past year. My 25(OH)D was 49 ng/ml in Sept 2020. I am now 18 weeks pregnant and just asked to have my levels measured again – down to 31 ng/ml (and my OB was resistant to measuring at first because I don’t have a history of deficiency – ugh). I’m attributing the 18 ng/ml decrease to both seasonal effects + increased need in pregnancy. Needless to say, I will be upping my dose!
Thanks for this post! Although I have a PhD in nutrition and can sort through literature, sometimes very practical advice around these issues is seriously lacking. Appreciate your work!
Thanks so much for this post, Lily! For the last years I’ve always been on the borderline of low vitamin D and now that I’m pregnant I’m not taking any risks and started supplementing with 4,000 IU. So far so good, levels are 32 ng/ml and expect them to rise a bit more.
Just one question: apart from taking the supplements with foods containing fats for better absorption, is there a better time to take them? Like first thing in the morning, at around noon, in the afternoon, at night…? Thanks again!
Thanks Lily! I’ve been taking a D3 + K2 supplement equating to about 3000 IU per day (D) which is 90mg of K2. Is there any issue with high K2 intake during pregnancy?
Hi Lily! I noticed in the Seeking Health vitamin D drops you recommend in this post only have 900 IU per serving. Do you recommend four drops/day to try to get closer to that 4000? Or finding a supplement that is 4000 IU? I am in my second tri, and live in San Francisco, so I most likely have a vitamin D deficiency! Thank you!
Have you ever come across anything in your research about Vitamin D3 supplements depleting Vitamin A/ retinol in the body?
Great article! My first baby has dental enamel issues so I’m going to really focus on Vitamin D this time around. I just checked my prenatal and the Seeking Health Optimal Prenatal also has 4000IU. I was happy to see that I’ve been getting that daily!
Hi Lily!
I would like your thoughts on Ritual Prenatal Multivitamins. Thanks a lot ☀️
Hi Lily! I’m looking for info regarding Vitamin K2 MK-4 doses during pregnancy. Do you know if there’s such thing as “too much?” I am taking Thorne’s liquid drops and they are 1 mg each. I was thinking of doing three drops a day but wondering your thoughts. I’ve heard MK4 is really important for fetal jaw and facial development. Thanks!!
Hi Lily! I love and live by your book Real Food for Pregnancy. While TTC, I read a lot about the benefits of raw milk and swapped my pasteurized milk for raw. Now, my midwife suggested I avoid raw milk and was wondering if you’ve found whether the benefits outweigh the risks. Would love to know your take!
I’m 12 weeks pregnant and have been supplementing with 5k ius for over year and just learned that my d is off the charts (99.3 ng/ml). I also get 1k ius from my prenatal. My midwife recommended ditching the extra 5k. It seems like research is limited do you have any insight into how bad that really was and the potential impact on baby?